

What is involved in using donor eggs?
Donor eggs are currently in very short supply worldwide with demand significantly outweighing supply. To ensure we provide high quality donors, we only source donors from reputable egg banks. This guide is intended to help you navigate the process of selecting a donor who is right for you.
Who is Egg Donation for?
Premature infertility: You may wish to use donor eggs if you have become prematurely infertile and your body is no longer producing eggs at all, or of a suitable quality for effective fertility treatment. This may occur if you have been diagnosed with early menopause or if you are undergoing or have undergone chemotherapy and/or radiotherapy for the treatment of cancer.
Advanced maternal age: Success rates for fertility treatment in women beyond the age of 42 using their own eggs are very low. In cases of advanced maternal age, you may choose to use donor eggs from a younger person to significantly improve your chances of becoming pregnant.
Genetic conditions: You may have been advised by a genetic counsellor and taken the decision not to have children naturally, or use your own eggs in fertility treatment, due to the risk of you passing on a genetic medical condition to any children born as a result of that treatment.
There are many medical, ethical, religious, legal and moral aspects which need to be considered. Some of these will be covered in consultation with the staff at Cambridge IVF before you embark on treatment. However, it is important that we highlight to you the need for everyone considering treatment with donor gametes to see a fertility specialist counsellor for implications counselling. At Cambridge IVF, implications counselling is mandatory before treatment can commence. This is to give you the opportunity to talk through all aspects of donor conception, to protect you and any future donor conceived children and to ensure you are making an informed decision. Information on our counselling services is available from our website.
What is the HFEA and why does it have to be involved?
The Human Fertilisation and Embryology Authority (HFEA) is the body that regulates fertility treatment in the UK. They license all clinics providing IVF and donor insemination, and keep a register of all licensed fertility treatments and children born as a result. This includes information about whether the treatment uses donated sperm, eggs or embryos.
What do I need to know before I choose my donor?
CMV
It is important that we know whether or not you carry a virus called Cytomegalovirus (CMV) when we are considering selection of a sperm or egg donor. CMV is one of the most common viral infections. It is estimated that around half of all adults in the UK have been infected by CMV. Most people develop the infection during early childhood or as a teenager and do not realise they have been infected as it causes few symptoms. Once you have been infected by CMV, the virus stays in your body for the rest of your life but does not usually cause you any further problems.
It is important however to understand that CMV can cause serious problems if a woman has her first CMV infection during pregnancy, as the infection can spread to the unborn baby (known as congenital CMV). It is estimated that 1-2 babies in every 200 will be born with congenital CMV in the
UK. Of these, only about 10% will experience issues, but they can be serious and include symptoms such as hearing loss and learning difficulties.
A simple blood test will tell you if you carry CMV. If the result of this test is POSITIVE, this shows that you already have the CMV virus and there is no risk of further viral exposure during pregnancy. This means you can select either a CMV positive or CMV negative egg or sperm donor for your treatment.
If your CMV result is NEGATIVE, you do not have the CMV virus and there is a risk that you could become infected by the virus during pregnancy.
The risk of passing on CMV through egg donation is negligible. On this basis, it is our policy that CMV negative egg recipients can select a CMV negative or a CMV positive egg donor. For use of a CMV positive donor however, we require informed consent from the egg recipient via a signed declaration that they wish to proceed with the specified CMV positive donor and are aware of the small risk involved in doing so.
If your CMV result is NEGATIVE and you also require donor sperm for your treatment, we recommend that you limit your sperm donor selection to donors who are clearly indicated as CMV NEGATIVE only. This is because the risk of viral contamination is higher (but still small) when using donor sperm compared to the use of donor eggs.
This may sound confusing but don’t worry, we are here to guide you through the process. We can even arrange for you to have the CMV blood test taken here at Cambridge IVF although we may have to charge you for this. Some GPs are happy to take a CMV blood test for you, so if you wish, you can enquire with your GP who may do this for you free of charge.
Who are the donors and how are they selected?
Fertility treatment in the UK is highly regulated by the HFEA and therefore donors recruited in the UK must meet the requirements of UK law. This also means that any donor eggs imported into the UK must also be compliant with UK legislation.
According to UK law, donors are aged 35 or under and have usually completed their own family. Donation is purely on a voluntary basis and no payment is made for this other than expenses incurred, with an upper limit specified by the HFEA.
Donors can be recruited in a number of ways:
Self-recruited donors: These are donors who are known to you, who are willing to donate their eggs to you.
Clinic or Donor Bank recruited donors: These are donors recruited by the clinic or donor bank. They may be egg sharers who need IVF treatment themselves and are donating some of their eggs to you, or altruistic donors who are donating all of their eggs.
How is the donor chosen?
All donors are screened thoroughly to ensure they are physically fit and free from diseases such as HIV and Hepatitis. Details of their height, weight, blood group, hair and eye colour are available so that you can match them with your characteristics.
How Does the Process Work?
Referral and initial consultation:
Before you can commence treatment, we will arrange an appointment to see you and your partner (if applicable). One of our Consultant Fertility Specialists will take you through the process to ensure that the treatment is appropriate and that your personal circumstances make you an appropriate egg recipient.
You will then see one of our Fertility Nurse Specialists who will complete the consent process and take a series of blood samples from you to test you for infectious diseases such as HIV and Hepatitis. The nurse will provide you with a characteristics form to complete with your characteristics for donor matching purposes. Where partner sperm is being used, a semen analysis is required so that we can check that there are enough sperm of suitable quality to allow us to fertilise the eggs using the appropriate procedure. It is advisable to arrange the semen analysis appointment in advance of the initial consultation, in order that the results can be made available to the Consultant at your appointment. In men over the age of 45 we also recommend the consideration of a sperm DNA fragmentation test prior to treatment. If this is relevant to you we will advise you and discuss this with you in more detail.
After this appointment, we advise you to arrange an appointment with a counsellor for implications counselling.
Selecting a donor – the process and timescale
Finding an appropriate donor can take some time due to the various considerations to be made when choosing a donor that you are comfortable with, and due to the low availability of donor eggs. For this reason we advise you to allow at least three to four months from your first appointment with us to the point at which you are ready to commence treatment. We will guide you through the process and ensure that any donor you choose is suitable for you.
Please also bear in mind that if you are undergoing treatment using frozen eggs, morally and ethically we cannot permit you to start your treatment until your donor eggs have arrived, been checked and are securely stored at Cambridge IVF.
We will do everything we can to assist you in finding an egg donor; however, it is important to be aware that due to the scarcity of donor eggs your treatment may be delayed or cancelled if a suitable donor is not available.
You should be aware that any child born as a result of treatment with donor gametes may inherit physical characteristics from the donor. This is most relevant where such physical characteristics are recessive and may not match you or your partners own characteristics (for example eye colour).
You should also be aware that the age limits for donation of sperm (45 years of age) and eggs (35 years of age) are in place to reduce the risk of age-related anomalies in the gametes provided. Despite these restrictions, you should be aware of the inherent decline in gamete quality associated with both the male and female aging process and that where donor age is nearing the age limit, the risk of genetic anomalies in any embryos created increases along with the risk of miscarriage following treatment.
There are two options for choosing a donor when undergoing treatment with Cambridge IVF:
Self-recruited (known) donors: These are donors who are known to you, who are willing to donate their eggs to you. If you are fortunate enough to have a willing egg donor, we will also arrange a separate consultation appointment for the donor and their partner if they have one. At this appointment one of our Consultant Fertility Specialists will take your donor through the process, take their medical history and complete consent forms appropriate to them to ensure that they are a suitable candidate. If eligible to donate, they will then also see a counsellor for implications counselling and one of our Fertility Nurse Specialists to complete their consent forms and commence the donor screening process.
Clinic or Donor bank recruited donors: These are donors recruited by Cambridge IVF or an external donor bank. They may be egg sharers (people who are undergoing IVF treatment themselves and are donating some of their eggs), or altruistic donors who are donating all of their eggs. Note that at this time Cambridge IVF are not recruiting donors locally but this may change in the future.
Cambridge IVF have partnered with Ovobank (www.ovobankid.com) an international donor bank to provide a pre-approved source of cryopreserved (frozen) donor eggs to our patients. We are only able to transfer in eggs that have been donated in accordance with the regulatory and screening requirements of the Human Fertilisation and Embryology Authority (HFEA).
Ordering eggs and transporting them to Cambridge IVF: Once you have selected your donor, we will check that the donor is appropriate for you and then you can proceed to place the order for the eggs directly with Ovobank. The eggs are transported to Cambridge IVF via a specialist cryogenic courier in a device called a ‘dry shipper’ which is designed to maintain ultra-low temperature (-196oC) for up to 21 days. When the eggs arrive in Cambridge, we carefully unpack them, check all of the details are correct and load them into one of our cryogenic storage devices where they will remain in storage until you wish to start your treatment cycle.
How many eggs should I order?
We recommend you order a minimum of 6 eggs for a single treatment cycle. There is significant attrition during the process which means it is very unlikely all 6 eggs will survive, fertilise and form embryos of suitable quality for use in treatment or cryopreservation. As a rough guide:
- 90% of frozen eggs will survive the warming process
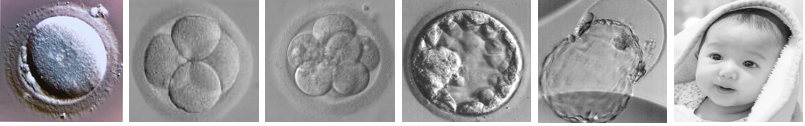
- 60% of those eggs which survive will fertilise and start to form embryos
- 50% of those embryos will form blastocysts on Day 5 or Day 6 of embryo culture (This is the advanced stage of embryo development where the embryo is ready to implant in the uterus and the stage at which we aim to do the embryo transfer).
- Given the above rates, the expected outcome from 6 eggs would be 1 blastocyst and less commonly 2 blastocysts.
(If your intention is to generate more blastocysts than you would use in a single cycle of treatment, (Usually 1 or 2.) you may want to consider purchasing more than six eggs initially and we are happy to discuss this with you).
We aim to freeze any additional embryos (not transferred) of suitable quality at the blastocyst stage 5 or 6 days after fertilisation occurred, using a vitrification technique similar to that used to initially store the eggs. The success rates from using frozen / thawed embryos do not vary statistically from those using fresh embryos so we are able to extend your treatment options beyond one embryo transfer using this strategy, thus minimising the need to source additional donor eggs should you wish or need to have a second embryo transfer.
What next?
Once you have found your egg donor and the eggs are transported to Cambridge IVF, you are ready to commence treatment.
If you are using a known donor, we will use medication to synchronise yours and your donor’s cycles in order that once the eggs have been collected from the donor and embryos created, an embryo can be transferred to you at the correct time of your cycle. If you would prefer to freeze your donor’s eggs or create embryos and freeze them for quarantine, there is no need to synchronise your cycles.
If you have opted to use cryopreserved donor eggs we will give you medication and monitor your cycle to thaw the eggs at the time that you would be ovulating naturally.
What happens after thawing donor eggs?
After warming the eggs we then need to try and fertilise them. When working with frozen eggs we have to attempt to fertilise your eggs using a procedure called Intracytoplasmic-sperm-injection (ICSI). During ICSI we select a single healthy sperm and manually inject it into the middle of the egg. Please be aware that ICSI treatment is required when using frozen-thawed eggs in treatment. This is because studies have demonstrated that the shell surrounding the egg hardens during the freezing process and can therefore prevent the sperm from entering the egg. We can overcome this problem by using ICSI. More information on ICSI is available to you in our separate patient information sheet via the Fertility Consents online platform.
If we are using fresh eggs from a known donor we will carry out the surgical egg collection to retrieve the eggs and then inseminate them using sperm. The method of insemination used (IVF or ICSI) will depend on the quality of the semen sample on the day that treatment is performed.
Once fertilisation is achieved the embryo/s will be cultured in a special incubator called an EmbryoScope in the laboratory for up to 6 days. Embryo transfer will typically be performed on day 5 and any remaining suitable quality blastocysts can be frozen for your future use on day 5 or day 6. Frozen embryos can be used in a future frozen embryo replacement cycle to further extend your treatment options.
Embryo transfer and embryo freezing processes performed for fresh or frozen donor eggs are exactly the same as those we routinely perform for all other treatment cycles. More information about this will be given to you during your consultation and via the Fertility Consents online platform.
What happens to the embryos if they are not frozen?
After assessment on day 6, any embryos that are not suitable for freezing are removed from culture and then they are discarded.
What is my chance of a successful outcome using frozen eggs?
Studies have demonstrated that your chance of a successful outcome using frozen-thawed eggs is the same as that using fresh eggs in ICSI treatment. Of course, in your case, the biological age of your eggs will, in most cases, be younger than you at the time of treatment. This should increase your chance of a successful outcome compared to other women in your age group using their own fresh eggs.
Are eggs harmed by being frozen?
Evidence from both published articles and from Cambridge IVF suggests that in excess of 90% of the eggs will survive the freezing and thawing process.
What are the risks to me and any resultant child when using donor eggs?
The main risk to you and any resultant child when undergoing treatment with donor eggs is the risk of transmission of genetic and infectious conditions. Under UK law, all approved donors must be rigorously screened for infectious and genetic diseases prior to acceptance. In all cases, donors must be screened for the following conditions as a minimum:
- HIV 1 & 2
- Hepatitis B Hepatitis C Syphilis HTLV 1&2
- Gonorrhoea Chlamydia Cystic Fibrosis
- Karyotype (Genetic screening)
Despite these stringent checks, we can never rule out the possibility that a donor may be the carrier of a genetically inheritable condition which may only come to light after you have received your treatment. In situations where this information is presented to us by Ovobank following your treatment we will contact you to inform you and explain the implications of the information we have received.
If you choose to undergo treatment using a known donor with fresh eggs rather than cryopreserved eggs, you should be aware that that it is not possible to quarantine the eggs to complete infection screening. Some infections can only be detected after an incubation period. This means that eggs which are frozen can remain in quarantine until the donor has been re-screened once the incubation period has passed. With fresh egg donation, quarantining eggs and re-screening the donor is not possible and therefore the potential risk of infection is increased. Alternatively, you may choose to freeze your donor’s eggs, or create embryos from the eggs and freeze those, in order to be able to rescreen the donor following the quarantine period and therefore reduce the risk of infection.
What are the risks to a child born using frozen eggs?
There is no evidence that any babies resulting from thawed eggs have an increased risk of harm or abnormality or that the pregnancy itself is at more risk because a frozen / thawed egg has been used. Cambridge IVF constantly monitors our results and pass on information to the HFEA which allows high power data analysis to be carried out at a national level to ensure that we continue to operate safely and in as informed an environment as possible.
Could anything go wrong with our storage?
Cambridge IVF has a state of the art cryostorage facility on site. Eggs are stored at very low (-196oC) temperatures using liquid nitrogen.
We do everything we can to maintain a high quality cryostore. We have a system in place that continually monitors the cryostore and will alert us immediately if there is the slightest suggestion of a problem. We use high security storage devices (known as straws) to reduce the theoretical risks of cross contamination between samples. Even with our exacting standards and commitment to quality in everything we do, we cannot provide a guarantee that your stored eggs may not be affected in the event of an ‘act of god’, civil disturbance, catastrophic equipment failure or any other unexpected and abnormal occurrence which may affect our service or facilities.
What are the costs involved?
Full financial information is available upon request or via our website Cambridge IVF Prices (opens in a new tab)
When should I tell my child about their origins and what should I say?
Before undergoing any treatment involving donor gametes (sperm, eggs or both) you will with no doubt have thought carefully about the various aspects of having a child. You might consider such matters as whether, how, and when you will tell any potential child about his or her origin using donor gametes.
There are no hard and fast rules about the best time to tell your child, but many experts say that it is better to start early, even before your child can talk or understand the facts of life. This allows you to become familiar with talking to your child about how they were conceived so that, by the time they are old enough to ask questions, it is already an accepted part of their life story.
We collect identifying information including the name and address of the donor at the time of donation and this is submitted to the HFEA as part of the donor registration process. Any child born as a result of the use of donated gametes has access to this full set of information including identifying information from the age of 18 (or to a non-identifying set information pertaining to genetic siblings from the age of 16 should they wish to marry) if they request this in writing from the HFEA.
This information will include:
- Physical description (height, weight and colour of eyes, hair and skin)
- Year and country of birth
- Ethnicity
- If the donor had any genetic children at the time of donation Their marital status
- If they were themselves conceived using donor gametes (if known) Skills
- Reason for donating
- Goodwill message for offspring Pen portrait of themselves
- Any other information the donor wished to pass on (e.g. occupation)
And for children over the age of 18 will also include;
- Full name
- Date, town and district of birth
- Last known postal address at the time of donation
- Identifying information about genetically related siblings (with mutual consent)
Equally the donor themselves is allowed to request information on the number, sex and year of birth of any resultant children but no identifying information is given to the donor regarding the children born using their gametes.
Donors are encouraged to provide detailed information including a short description of themselves and a message of goodwill to any children conceived. This will be made available to you, and you may find this helpful once your child starts to ask detailed questions. It is a good idea to talk to the clinic about how you could approach telling your child. The Donor Conception Network (opens in a new tab) also offer advice and information leaflets and personal stories from other people who have been through the same process you are considering.
Will the child be legally mine? What do I put on the birth certificate?
If you and your partner were treated together at a licensed fertility clinic in the UK and have accurately completed the appropriate consent forms, you are the legal parents of the child and should put your names on the birth certificate. The donor has no legal relationship or financial responsibilities towards the child. The change in the law on anonymity does not affect this.
Information regarding legal parenthood following donor gamete treatment can be complex and this information should be read in conjunction with our legal parenthood information for patients. It is important to ensure that your wishes are correctly represented in your consents to ensure that there is no confusion over the legal status of the parents after the birth of the child.
Can I use eggs for future siblings so my children have the same genetic origins?
You can if more eggs are available, though due to the current scarcity of donor eggs this is unlikely. You may be in the lucky situation where you have surplus embryos available after your embryo transfer. If this is the case, we will culture those embryos to the blastocyst stage. If any of them form good quality blastocysts we will cryopreserve them for your future use, provided both the egg and sperm provider have consented to embryo freezing.
Is there anyone else who knows how I /we feel?
We know from experience how stressful your treatment can be and how this can affect relationships. We offer a counselling service to provide you with any additional support you feel you may need.
Please telephone us to arrange an appointment.
There are also several support groups that may help.
- Fertility Network UK (opens in a new tab). The largest network in the UK offering information and advice. It has groups throughout the country and also produces a range of publications on infertility. Tel: 08701 188088.
- Donor Conception Network (opens in a new tab). A national support group for people who have conceived through donation and those considering it. They can give you advice and support and also the chance to meet parents with donor-conceived children. Call 020 8245 4369
- Fertility Friends (opens in a new tab). An online information and support website for those undergoing fertility treatment.
We hope you have found this booklet informative and interesting. We realise we may not have covered all of your questions so if you do have any other queries, we are here to help so please contact us via any of the means below:
Cambridge IVF Kefford House Maris Lane Trumpington Cambridge CB2 9LG
Switchboard: 01223 349010
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

