
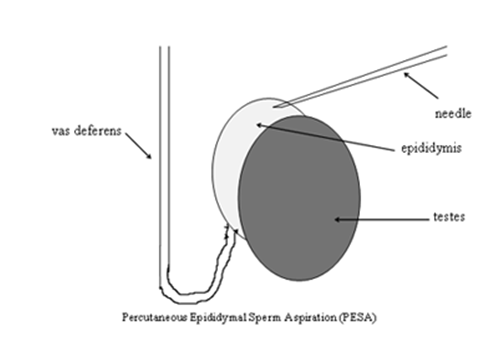
Sperm collection from vas deferens or epididymis for use in artificial fertilisation (PESA).
This procedure is usually performed for patients who do not have any sperm within the ejaculate due to a blockage of some kind, which may be due to prior surgery such as a vasectomy (obstructive azoospermia).
In most cases sperm will be found from your PESA procedure and will be frozen for your future use to fertilise eggs harvested from your partner using In Vitro Fertilisation (IVF) with or without Intracytoplasmic Sperm Injection (ICSI). ICSI is an extension to the standard IVF technique. Using the ICSI technique, a single living sperm is identified, immobilised and injected into each available egg. The need for the use of ICSI will depend on the number, motility and morphology of the sperm harvested and frozen during your PESA procedure. Some of the eggs fertilised by IVF or ICSI will then form embryos which can be transferred back to your partner to attempt a pregnancy.
Please note that we will not be able to freeze any sperm we may find until we have the results for your HIV, Hepatitis B and Hepatitis C antibody tests. If you should test positive for any of these conditions we have dedicated and separate long-term cryogenic storage devices available on site so we can store your samples whatever the results of your viral blood tests might be.
What are my options if PESA is unsuccessful?
If it is not possible to find sperm with the PESA procedure, then testicular sperm aspiration or extraction may be performed during the same operation. This is the case in about 1 in 10 cases overall.
What happens during the procedure?
You will be admitted on the same day as your surgery. You may receive an appointment for pre-assessment before your admission, to assess your general fitness, to screen for the carriage of MRSA and to perform some baseline investigations.
You will be asked not to eat or drink for 6 hours before surgery and immediately before the operation.
The procedure may be performed under local anaesthetic or a full general anaesthetic (where you will be asleep throughout the procedure). All methods used will minimise any pain; your surgeon or anaesthetist will explain the benefits and risks of each type of anaesthetic to you.
The operation is usually performed either through a small incision in the scrotum or by simply puncturing the skin with a small needle. The fluid aspirated from the needle is passed to the laboratory team and examined under the microscope for the presence or absence of sperm.
Multiple samples may be taken from both testicles until sufficient sperm have been harvested for freezing for your future treatment needs.
Are there any side effects?
- A small amount of scrotal bruising
- No guarantee that sperm will be obtained
- No guarantee that pregnancy will be achieved
- Worsening obstruction of the vas deferens or epididymis
- Infection and/or bleeding in the scrotum or epididymis requiring surgical evacuation
- In the unlikely event that you have problems passing urine after the procedure you may need to have a catheter inserted into your bladder temporarily.
- Please note that there is a high chance but no guarantee of finding sperm.
What happens immediately after the procedure?
You may experience discomfort for a few days after the procedure but painkillers will be given to you to take home. If stitches are used they will be absorbable and do not require removal.
The procedure is done as a day case. You will be allowed home after you have passed urine. Your ice pack should be removed from your scrotal support before you leave. The dressings should stay in place for 24 hours after the procedure, and after this can be carefully removed.
What should I expect when I get home?
You are advised to rest for the first 48 hours at home. You should wear your scrotal support for 1-2 weeks depending upon any discomfort you experience. You will usually need 3-4 days off work, but not more unless you have a manual job, in which case 7-10 days may be needed.
Over the first few days, the scrotum and groin may feel uncomfortable and bruised. The skin sutures (if used) do not need to be removed and will usually drop out after a couple of weeks; occasionally, they may take slightly longer to disappear. Do not try and remove them yourself.
You should avoid sexual intercourse until you feel completely comfortable.
If you require any further information then please get in touch with us on the number below.
What else do I need to know?
All men will benefit from following basic lifestyle advice, which includes:
- Stopping smoking
- Participating in regular moderate exercise
- Considering taking steps to lose weight if your BMI exceeds 25
- Avoiding saunas, steam rooms, hot tubs and bathing in hot water
- Avoiding wearing tight clothing and underwear which compressed the testicles against the body
- Eating healthily: plenty of fruit, vegetables, nuts, beans and pulses.
Men may also take a make fertility supplement. The supplement we recommend is the Vitabiotics ‘Wellman Conception’ range. These can be purchased over the counter from any pharmacy. Ideally you should take these for three months prior to any operation to try and retrieve sperm.
You should avoid travelling for three months to any Zika infected area prior to your sperm retrieval.
Patients should note that while the procedure aims to obtain sperm which can then be used with IVF/ ICSI, sometimes insufficient healthy sperm may be retrieved. It is therefore possible that, on the day of your partner’s egg collection, the laboratory team may need to use one of a range of techniques to either try to ‘wake the sperm up’ or to identify immotile sperm which are alive for selection for the ICSI procedure. In such cases it is likely that the number of eggs which fertilise will be lower. If our laboratory team are unable to identify any sperm suitable for use in ICSI on the day of treatment we will recommend the freezing of your partners’ eggs and a review appointment with a member of the clinical team to review and discuss your options. Each of these other processes may have their own consent processes which will be discussed with you in advance of your procedure.
How to get in Touch
Cambridge IVF
Kefford House
Maris Lane
Trumpington
Cambridge
CB2 9LG
Follow us on
- Twitter - @cambridgeivf (opens in a new tab)
- Instagram - @cambs_ivf (opens in a new tab)
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

