What is the evidence base for this information?
This leaflet includes advice from consensus panels, the British Association of Urological Surgeons, the Department of Health and evidence based sources; it is, therefore, a reflection of best practice in the UK. It is intended to supplement any advice you may already have been given by your Urologist or Nurse Specialist as well as the surgical team at Addenbrooke’s. Alternative treatments are outlined below and can be discussed in more detail with your Urologist or Specialist Nurse.
What does the procedure involve?
Self-injection of alprostadil to produce a penile erection sufficient for intercourse.
What are the alternatives to this procedure?
Tablet treatment, vacuum erection assistance devices, penile prostheses, MUSE, psychosexual counselling, no treatment.
What should I expect before the procedure?
Penile injections do not require any form of anaesthetic and are usually performed in outpatients under the supervision of a consultant Urologist or a Specialist Nurse.
The technique of penile injection produces the most natural form of erection for a man with impotence. This technique can allow the return of normal sexual activity although, if you have problems with ejaculation, these are unlikely to be helped by this method.
For your first injection, prepare 5μg of alprostadil using the dual chamber device.
This ingenious device allows the dose to be selected, the drug to be mixed with fluid and the injection to be given using the same syringe and needle. Your Specialist Nurse will show you how to use the device on the first occasion.
Please be sure to inform your Urologist in advance of your surgery if you have any of the following:
- an artificial heart valve
- a coronary artery stent
- a heart pacemaker or defibrillator
- an artificial joint
- an artificial blood vessel graft
- a neurosurgical shunt
- any other implanted foreign body
- conditions that might predispose to priapism, such as sickle cell anaemia or trait, multiple myeloma, or leukaemia;
- anatomical deformation of the penis, such as angulation, cavernosal fibrosis, or Peyronie's disease
- prescription for blood thinning medication such as warfarin, aspirin, rivaroxaban, dabigatran, apixaban, edoxaban, clopidogrel or ticagrelor
- medication for treating high blood pressure (anti-hypertensives)
- medicines used for respiratory and heart disease (sympathomimetics)
- medicines that widen blood vessels (vasodilative agents)
- other medicines for erectile dysfunction such as sildenafil or papaverine
- a previous or current MRSA infection
- high risk of variant CJD (if you have received a corneal transplant, a neurosurgical dural transplant or previous injections of human derived growth hormone)
What happens during the procedure?
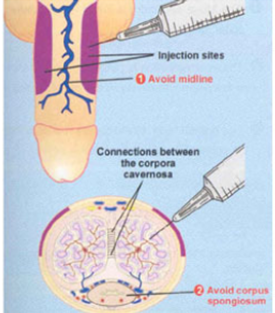
Insert the needle into the side of the penis with a sharp thrust, pushing it in to its full depth. The injection should be given about one inch (two and a half cm) behind the circular ridge (corona) which forms the head (glans) of the penis. Try to avoid piercing veins running directly under the skin. Do not give injections into the under surface (where the urethra is at risk) or on top of the penis (where large veins are at risk).
Initial insertion of the needle is, of course, slightly painful but a firm and rapid thrust improves or minimises the pain of needle insertion. You may experience a slight pricking sensation on injection which is not unusual. If there is severe pain, stop the injection immediately and seek medical advice if the pain does not settle within 30 minutes.
What happens immediately after the procedure?
When the contents of the syringe have been injected, remove the needle and use your finger or thumb to put gentle pressure on the injection site for a few minutes. Gently massaging the penis a few times between thumb and finger will help distribute the drug throughout the penis.
A satisfactory erection should be achieved within 10 minutes. Your first erection using this technique normally lasts for about 45 minutes. The nurse practitioner will adjust the dose as necessary.
Are there any side effects?
Most procedures have a potential for side‑effects. You should be reassured that, although all these complications are well recognised, the majority of patients do not suffer any problems after a urological procedure.
Please use the check boxes to tick off individual items when you are happy that they have been discussed to your satisfaction:
Common (greater than one in 10)
- Pain / discomfort at the time of injection
- Bruising under the skin of the penis after injection
- A persistent painful erection lasting longer than 4 hours (10%)
Occasional (between one in 10 and one in 50)
- Scarring or bending of the penis on erection following repeated injections given at the same site
- Failure to achieve an erection following injection
- Bleeding from the water pipe (urethra) due to a misplaced injection
- Progressive lack of response to injections due to scarring within the penis
Rare (less than one in 50)
- Infection at the injection site (more likely if you are diabetic)
- Hospital-acquired infection (overall risk for Addenbrooke’s)
- Colonisation with MRSA (0.01%, two in 15,500)
- Clostridium difficile bowel infection (0.02%; three in 15,500)
- MRSA bloodstream infection (0.00%; 0 in 15,000)
(These rates may be greater in high risk patients eg with long term drainage tubes, after removal of the bladder for cancer, after previous infections, after prolonged hospitalisation or after multiple admissions.)
What should I expect when I get home?
Your erection may last anything from five minutes to two hours. If your erection lasts more than four hours or becomes very painful, you should contact the Urology staff at Addenbrooke's immediately; they will arrange for an antidote to be administered to bring your erection down but this must be given in hospital.
Please contact your doctor if you develop severe pain or bleeding.
What else should I look out for?
You may develop a small bruise (haematoma) under the skin of the penis at the site of injection. This is nothing to worry about and will disappear by itself over the next few days. If it becomes very large, please seek medical advice.
Are there any other important points?
You are advised not to use this technique for obtaining erections more than three times in any one week and injections should not be used more than once in any one day. More frequent injections run the risk of damaging the erectile tissue of the penis (which can make you impotent again) and of producing long lasting painful erections.
Although this technique is well tried and tested, the long term effects of repeated injections of alprostadil are not yet known accurately. However, many thousands of patients worldwide are using this technique without problems.
If the dose of drug produces no erection, you should contact the erectile dysfunction specialist nurse who will arrange for you to be re-assessed in the outpatient department.
It is important to dispose of your needles safely; your local pharmacy can advise you about this.
Injection of alprostadil can start a small amount of bleeding where the needle enters. This could increase the risk of transmission of such diseases. Condoms can protect against sexually transmitted diseases. If you need advice about contraception or ‘safe sex’ speak to your doctor or contact your local family planning clinic.
Driving after surgery
It is your responsibility to ensure that you are fit to drive following your surgery.
You do not normally need to notify the DVLA unless you have a medical condition that will last for longer than three months after your surgery and may affect your ability to drive. You should, however, check with your insurance company before returning to driving. Your doctors will be happy to provide you with advice on request.
Privacy and dignity
Same sex bays and bathrooms are offered in all wards except critical care and theatre recovery areas where the use of high tech equipment and/or specialist one to one care is required.
Hair removal before an operation
For most operations, you do not need to have the hair around the site of the operation removed. However, sometimes the healthcare team may need to remove hair to allow them to see or reach your skin. If the healthcare team consider it is important to remove the hair, they will do this by using an electric hair clipper, with a single-use disposable head, on the day of the surgery. Please do not shave the hair yourself, or use a razor for hair removal, as this can increase the risk of infection to the site of the operation. If you have any questions, please ask the healthcare team who will be happy to discuss this with you.
References
NICE clinical guideline No 74: Surgical site infection (October 2008); Department of Health: High Impact Intervention No 4: Care bundle to preventing surgical site infection (August 2007)
Caverject solution for injection patient information leaflet. Pfizer limited. Last updated on eMC 24-May-2017.
Is there any research being carried out in this field at Addenbrooke’s Hospital?
There is no specific research in this area at the moment but all operative procedures performed in the department are subject to rigorous audit at a monthly audit and clinical governance meeting.
Who can I contact for more help or information?
Oncology nurses
Uro-oncology nurse specialist
01223 586748
Bladder cancer nurse practitioner (haematuria, chemotherapy and BCG)
01223 274608
Prostate cancer nurse practitioner
01223 274608 or 216897 or bleep 154-548
Surgical care practitioner
01223 348590 or 256157 or bleep 154-351
Non-oncology nurses
Urology nurse practitioner (incontinence, urodynamics, catheter patients)
01223 274608 or bleep 154-594
Urology nurse practitioner (stoma care)
01223 349800
Urology nurse practitioner (stone disease)
07860 781828
Patient advice and liaison service (PALS)
Telephone: +44 (0)1223 216756
PatientLine: *801 (from patient bedside telephones only)
Email PALS
Mail: PALS, Box No 53
Addenbrooke's Hospital
Hills Road, Cambridge, CB2 2QQ
Chaplaincy and multi faith community
Telephone: +44 (0)1223 217769
Email the chaplaincy
Mail: The Chaplaincy, Box No 105
Addenbrooke's Hospital
Hills Road, Cambridge, CB2 2QQ
MINICOM System (‘type’ system for the hard of hearing)
Telephone: +44 (0)1223 217589
Access office (travel, parking and security information)
Telephone: +44 (0)1223 596060
What should I do with this leaflet?
Thank you for taking the trouble to read this patient information leaflet. If you wish to sign it and retain a copy for your own records, please do so below.
If you would like a copy of this leaflet to be filed in your hospital records for future reference, please let your Urologist or Specialist Nurse know. If you do, however, decide to proceed with the scheduled procedure, you will be asked to sign a separate consent form which will be filed in your hospital notes and you will, in addition, be provided with a copy of the form if you wish.
I have read this patient information leaflet and I accept the information it provides.
Signature……………………………….……………Date…………….………………….
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

