Some useful post-operative advice
You have now undergone an operation to remove the worn out sections of your hip joint, replacing them with new metal and plastic parts. The advice that is provided for you within this booklet will help you to make a speedy recovery, along with directions provided to you by your physiotherapy, nursing and surgical team.
You will be referred to ……………………………………………… for onward Physiotherapy. Tel no: …………………………………
Cambridge Movement Surgical Hub Physiotherapy
Tel No: 01223 388160
Ward D8/C8 Physiotherapy Tel No: 01223 216104
Specialist Orthopaedic Nurse Tel No: 07926 071532 (only for clinical issues up to 30 days after surgery)
Out-patient Helpdesk Tel No: 01223 806000/216231 (for issues with clinic follow up appointments etc)
The Elective “Pathway”
Recovering from hip replacement surgery has significantly changed over recent years. Early mobilisation has been shown to improve your recovery and reduce post-operative complications. Your pathway is based on our team’s expertise and we will support you to getting back on your feet. We aim to get you home as quickly as possible following your operation. You will be assisted by the physiotherapy and nursing staff on the day of your surgery to mobilise, and then the physiotherapy team will aim to see you twice a day thereafter to assist you with exercises and mobility. To enhance your recovery we encourage you to get up and mobilise frequently throughout the day using the walking aids we provide for you and to get dressed in your normal clothes.
- Do take your pain relieving medication, this will help your recovery
- Do the exercises you have been taught, at least 5 times a day
- Do increase your walking distance a little further each day
- Do make sure you have somewhere to rest if you get tired when walking
- Do watch your weight
- Do lie flat for half an hour twice a day to stretch the hip and to restore good posture
Sleeping
You may lie in bed however you feel comfortable. Many people prefer to lie on their backs for a while after a hip replacement, however you may lie on either side if it is comfortable. If you lie on the un-operated side it may be more comfortable to put a pillow between your legs.
Sitting
Make sure you sit on a comfortable but supportive chair that you can stand up from. Ideally the chair should have arms that you can push on to make standing up easier.
Walking
As you become steadier on your feet you can slowly increase the distance you walk and reduce the support you need from your walking aids. As you progress you may try general household activities, however try to avoid prolonged standing. If you wish to resume a particular hobby please discuss this with your surgeon or physiotherapist.
Post operation
The following information will help you during the first few months after your total hip replacement.
You may experience some surgical pain and discomfort from your new hip, this should settle with the help of pain relieving medication. The stiffness and soreness may last a few months until the muscles and structures around the hip have fully healed and strengthened.
You will be seen by a physiotherapist on the day of your surgery (unless you are very late back from theatre) who will encourage you to start gently exercising your new hip. You will be assisted out of bed, encouraged to walk with walking aids and helped to sit out in a chair next to your bed.
It is important to practise your exercises regularly, at least five times a day. The physiotherapist will encourage and help you to become fully independent around the ward and teach you to negotiate steps or stairs if needed.
You will also be seen by an occupational therapist who will advise you on any aids you may require to help you with independence in the home.
You will go home as soon as you are fit for discharge, staying in hospital longer than necessary comes with its own risks.
Healing
It usually takes:
- four to six weeks for the wound to heal
- six weeks for the ligaments and joint soft tissues to heal
- a further six weeks for them to strengthen
- up to six months for the bone and muscles to fully heal and strengthen
Your progress
Everybody recovers at different rates depending upon your age, general health and the nature of your surgery. There is no set timetable. But it is important to understand that your recovery in hospital requires your input as much as that of the hospital staff.
Early exercise and mobility are key to a successful result and hopefully a short hospital stay. Practise your exercises five times a day. Remember “motion is the lotion”
Breathing exercises
These will help you recover from the anaesthetic and make you more alert. If you have chest problems such as asthma or bronchitis it is even more important for you to do these exercises to reduce the risk of a chest infection.
- Relax your shoulders and upper chest
- Take a deep breath in through your nose
- Hold the breath for four seconds, then breathe out through your mouth
- Following the fourth breath, cough deeply from the belly (do not just clear your throat)
Try to do this every hour during your stay in hospital.
Circulation and strength exercises
Detailed below are exercises that you can practise with the guidance of your physiotherapist. It is important to keep your circulation moving. Vigorous, rhythmic pumping of the calf muscles in the lower leg will help you to do this. See in particular the first two exercises below.
- Start by completing five repetitions of each exercise and, as you get stronger, increase the repetitions until you can manage twenty of each.
- Practice all the exercises shown five times a day.
- Once you are independently mobile with the use of walking aids, aim to stand and take a little walk every hour of the day that you are awake.
Exercises following total hip replacement
Please be aware that this leaflet is to be used as a guide. If you find these exercises painful, please seek advice from your physiotherapist or doctor.
Bed/lying exercises






Seated Exercises






Standing Exercises






If any of the exercises in this leaflet are causing you sharp unexpected pain, stop that exercise immediately and ask your physiotherapist for further advice, but please continue with all other exercises.
Use of ice
Ice can be used after your surgery to reduce pain and swelling. Wrap an ice pack in e.g. a clean damp tea towel to avoid direct contact with the skin. Apply to the hip for 20 minutes.
Negotiating stairs
The golden rules for walking up or down stairs are one step at a time and hold the rail in one hand.
How to go up stairs

How to come down stairs

Driving
You may travel as a passenger in a car as soon as you leave hospital and certainly to get home from the hospital.
You should not drive for at least six weeks or at your surgeon’s discretion. Break up long journeys hourly. When you are fit enough to drive again do not forget to tell your insurance company you have an artificial hip. It is important that you do not drive until you feel fully in control of the car in an emergency situation, i.e. you can perform an emergency stop without hesitation. This is usually after 6 weeks or after you have seen your surgeon at your follow up.

- Slide the passenger seat back on its runners to give maximum leg room.
- Sit onto the side of the seat facing out of the door.
- Slide your bottom back towards the centre of the car.
- Lift your legs into the foot well whilst swivelling yourself round so you are facing forwards.

- Slide the seat back.
- Turn towards the outside, lifting each leg out into the gutter, whilst swivelling yourself round.
- Stand up.
NB: You will be referred to your local physiotherapy service on discharge. They will progress your exercises as and when appropriate.
Pain relief
To help with your treatment, it is important that you have adequate pain relief. If you are suffering high levels of pain following discharge from hospital, please seek advice from your General Practitioner (GP). We want your pain to be under control enough so you can mobilise and do your exercises regularly.
Progression once you have gone home
Physiotherapy after you leave hospital is now very limited due to current pressures on the health system, so in this section we aim to give you as much advice as possible to help you progress yourself back to the level you want to reach. You can split up the exercises to fit in with your day e.g. do the seated ones when you are sitting in a chair anyway, the lying ones in the morning when you are still in bed or when you are on your bed having a rest etc.
At two weeks
Continue with all the exercises you were given in hospital but do more repetitions if you feel able, e.g. move from 10 of each to 20.
Remember moving your new hip joint keeps it from becoming stiff.
At around two weeks you should be going to your GP Practice nurse to have the dressing removed, the wound checked and any clips or stitches taken out if needed. They will tell you whether you can now start to shower. Getting in and out of a bath will still prove difficult.
The hip may still be sore especially at the end of the day but some people will be off the stronger pain killers by now.
You may still have swelling around the hip or even lower down your leg, this is perfectly normal. Continue to use ice packs if you have found it helpful and try to take a rest with your legs up at least once a day.
You should be able to do most of your normal light activities around the home, e.g. make a cup of tea or a simple meal.
You should be increasing your mobility distance by a small amount each day. Weather permitting you should be trying to take gentle walks outside. Take someone with you for confidence.
Some people who went home on crutches will be dropping down to one crutch around the two week mark. The one crutch should be in the hand on the opposite side of the new hip and the crutch is put forward at the same time as the operated leg. As soon as you feel able you can stop using walking aids altogether. Crutches were to lean on to take pressure off the new hip but ideally you should be using your own muscles to balance when walking as soon as possible.
If you were using a walker or frame before your hip surgery, progression may take longer and of course some patients may need their walking aids permanently for other reasons.
At six weeks
If you feel able to perform an emergency stop without hesitation and are off strong painkillers, most people can return to driving at about six weeks. If in doubt talk to your GP or surgeon at your follow up appointment and inform your insurance company.
Walking is one of the best exercises you can do, gentle enough on the new hip but increases muscle strength, balance and stamina.
Start to do the more advanced exercises below when you feel able to. Regular exercise helps recover normal hip movement, gets good muscle strength and will allow you to return to the activities you want to be able to do.
Side lying hip abduction

The Clam

Prone hip extension

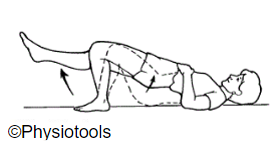
Bridge with hip adduction

Single leg bridge
Sit to stand

Step Ups

Balance-Tandem Walking

Balance-Side stepping

Balance-Single leg stand

At twelve weeks
Most patients really feel back to themselves again at this point, although improvements can continue for over a year. Keep on doing your exercises. Most patients can walk without aids.
Most pain and swelling should have gone, you can likely do most of your regular day to day activities, e.g. gardening, light housework, longer walks, dancing etc.
At six months almost all patients are greatly improved but may not have full stamina. Keep doing the exercises in this booklet for strength and lifestyle exercises for general health and fitness, e.g. yoga, pilates, swimming.
For specific sports please discuss with your surgeon. High impact sports or activities like running, jumping or lifting heavy weights should be avoided though.
Contact information
If you have any concerns following discharge from hospital, the inpatient physiotherapy team can be contacted on 01223 388160 (Cambridge Movement Surgical Hub) or 01223 216104 (Ward D8/C8)
Information
Please be aware that this leaflet is to be used as a guide. If you find these exercises painful please seek advice from your physiotherapist or doctor.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

