What is the evidence base for this information?
This leaflet includes advice from consensus panels, the British Association of Urological Surgeons, the Department of Health and evidence based sources; it is, therefore, a reflection of best practice in the UK. It is intended to supplement any advice you may already have been given by your urologist or nurse specialist, as well as the surgical team at Addenbrooke’s. Alternative treatments are outlined below and can be discussed in more detail with your urologist or nurse specialist.
What does the procedure involve?
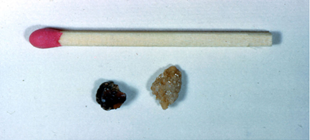
This involves the administration of shockwaves through the skin to fragment urinary tract stones into small enough fragments to pass naturally. The procedure involves either x-ray or ultrasound scanning to localise the stone(s).
What are the alternatives to this procedure?
Telescopic surgery, open surgery, observation to allow spontaneous passage.

What should I expect before the procedure?
You will usually be admitted on the same day as your treatment. It may be useful to bring your own dressing gown to wear over your hospital gown. On arrival, an x-ray may be taken to confirm the presence of your stone(s).
You may have a light meal on the morning of your treatment but you should drink only clear fluid in the two to four hours before the treatment. Please inform the nursing staff of the person who will be driving you home. We may give you an injection of a strong painkiller or an anti-inflammatory suppository once you arrive in the clinic.
Please be sure to inform your Urologist in advance of your surgery if you have any of the following:
- an artificial heart valve
- a coronary artery stent
- a heart pacemaker or defibrillator
- an artificial joint
- an artificial blood vessel graft
- a neurosurgical shunt
- any other implanted foreign body
- a prescription for warfarin, aspirin, rivaroxaban, dabigatran, apixaban, edoxaban or clopidogrel, ticagrelor or blood thinning medication
- a previous or current MRSA infection
- high risk of variant CJD (if you have received a corneal transplant, a neurosurgical dural transplant or previous injections of human derived growth hormone)
What happens during the procedure?
Normally, no anaesthetic is necessary and you will be awake throughout the procedure, but children usually require a general anaesthetic.
The treatment will be monitored by a nurse and a lithotripsy technician. The shock waves can cause deep discomfort in the kidney and a sensation of being flicked with an elastic band on the skin of your back. If this proves excessively painful, additional painkiller and sedation can be administered during the treatment. Treatment normally lasts between 30 and 60 minutes, depending on the size of your stone(s).

What happens immediately after the procedure?
You will normally be taken back to a side room to recover. The specialist nurse will also perform routine post-operative checks. As soon as you have recovered from the treatment, you will be able to go home. Painkillers will be given to you before your discharge. The average hospital stay is two to four hours.
Are there any side effects?
Most procedures have a potential for side effects. You should be reassured that, although all these complications are well recognised, the majority of patients do not suffer any problems after a urological procedure.
Please use the check boxes to tick off individual items when you are happy that they have been discussed to your satisfaction:
Common (greater than one in 10)
☐ Bleeding on passing urine for a short period after the procedure.
☐ Pain in the kidney as small fragments of stone pass after treatment (20%).
☐ Urinary tract infection due to bacteria released from the stone during fragmentation, requiring antibiotic treatment (10%).
☐ Bruising or blistering of the skin in the loin or on the front of the abdomen.
☐ Need for repeated ESWL treatments (15 to 20%).
☐ Failure to fragment very hard stone(s) requiring an alternative treatment (less than approximately 14%).
Occasional (between one in 10 and one in 50)
☐ Severe infection requiring intravenous antibiotics (less than 1%) and sometimes drainage of the kidney by a small drain placed through the back into the kidney.
☐ Stone fragments occasionally get stuck in the tube between the kidney and the bladder, requiring hospital attendance and, occasionally, surgery to remove the stone fragments.
Rare (less than one in 50)
☐ Kidney damage (bruising) or infection needing further treatment.
☐ Recurrence of stones (less than 1%).
What should I expect when I get home?
When you get home, you should drink twice as much fluid as you would normally to flush your system through and minimise any bleeding or infection. Painkillers should be taken as necessary.
Some blood in the urine is normal for 48 to 72 hours. If you develop bruising/blistering in your loin or on your abdomen, simple skin creams will usually ease any discomfort and the bruising normally resolves within seven days.
What else should I look out for?
You should contact your GP immediately:
- If you develop a fever, severe pain on passing urine, inability to pass urine or worsening bleeding.
- If small blood clots or stone fragments pass down the ureter from the kidney, resulting in renal colic.
Are there any other important points?
You will be informed before your discharge of any follow-up arrangements. This will usually involve either further lithotripsy, operative surgery or a simple follow-up outpatient appointment when a further x-ray will be taken.
If you have a stent in place, you may be given an appointment for removal of the stent in the Day Surgery Unit under local anaesthetic if this is appropriate. You can prevent further stone recurrence by implementing changes to your diet and fluid intake. If you have not already received a written leaflet about this, contact your named nurse, the specialist nurse in outpatients or your consultant.
If you have any concerns please contact the specialist nurse on 07860 781828.
Driving after surgery
It is your responsibility to ensure that you are fit to drive following your surgery. You do not normally need to notify the DVLA unless you have a medical condition that will last for longer than three months after your surgery and may affect your ability to drive. You should, however, check with your insurance company before returning to driving. Your doctors will be happy to provide you with advice on request.
Privacy and dignity
Same-sex bays and bathrooms are offered in all wards except critical care and theatre recovery areas where the use of high tech equipment and/or specialist one-to-one care is required.
Hair removal before an operation
For most operations, you do not need to have the hair around the site of the operation removed. However, sometimes the healthcare team need to see or reach your skin and if this is necessary they will use an electric hair clipper with a single-use disposable head, on the day of the surgery. Please do not shave the hair yourself or use a razor to remove hair, as this can increase the risk of infection. Your healthcare team will be happy to discuss this with you.
References
NICE clinical guideline No 74: Surgical site infection (October 2008); Department of Health: High Impact Intervention No 4: Care bundle to preventing surgical site infection (August 2007)
Is there any research being carried out in this field at Addenbrooke’s Hospital?
There is no specific research in this area at the moment but all operative procedures performed in the department are subject to rigorous audit at a monthly audit and clinical governance meeting.
Who can I contact for more help or information?
Oncology nurses
Uro-oncology nurse specialist: 01223 586748
Bladder cancer nurse practitioner (haematuria, chemotherapy and BCG): 01223 274608
Prostate cancer nurse practitioner: 01223 274608 or 01223 216897
Surgical care practitioner: 01223 348590 or 01223 256157
Non-oncology nurses
Urology nurse practitioner (incontinence, urodynamics, catheter patients): 01223 274608
Urology nurse practitioner (stoma care): 01223 349800
Urology nurse practitioner (stone disease): 07860 781828
Patient advice and liaison service (PALS)
PALS, Box No 53, Addenbrooke's Hospital, Hills Road, Cambridge, CB2 2QQ
01223 216756
PatientLine: *801 (from patient bedside telephones only)
Email PALS
Chaplaincy and multi faith community
The Chaplaincy, Box No 105, Addenbrooke's Hospital, Hills Road, Cambridge, CB2 2QQ
01223 217769
Email the Chaplaincy
MINICOM System ('type' system for the hard of hearing)
01223 217589
Access office (travel, parking and security information)
01223 596060
What should I do with this leaflet?
Thank you for taking the trouble to read this patient information leaflet. If you wish to sign it and retain a copy for your own records, please do so below.
If you would like a copy of this leaflet to be filed in your hospital records for future reference, please let your urologist or specialist nurse know. If you do, however, decide to proceed with the scheduled procedure, you will be asked to sign a separate consent form which will be filed in your hospital notes and you will, in addition, be provided with a copy of the form if you wish.
I have read this patient information leaflet and I accept the information it provides.
Signature ……………………………….…………… Date …………….………………….
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

