

What is Cryopreservation?
Cryopreservation or ‘Freezing’ of embryos takes place on day 5 and 6 of your treatment cycle after your embryo transfer in cases where we have 1 or more good quality embryos remaining following your embryo transfer. It may also take place in cases where a ‘freeze-all’ has been advised by the medical team depending upon embryo quality.
By storing embryos we can then thaw them out and transfer them back to you in the same way as we did in your ‘fresh’ treatment cycle. Freezing and thawing of embryos allows us to extend the number of chances you have to become pregnant from one egg collection procedure.
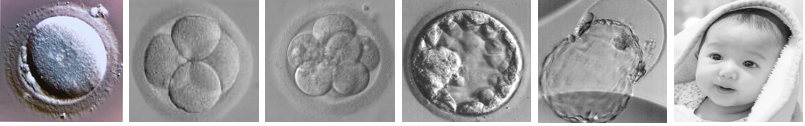
At Cambridge IVF we use a technique called ‘vitrification’ to rapidly freeze any good quality blastocysts (advanced day 5 or day 6 embryos) which are remaining after your embryo transfer procedure. Any embryo which has the capacity to form a good quality blastocyst certainly has the potential to form a pregnancy. We freeze using this technique at the blastocyst stage as evidence suggests that vitrification is the most effective method to successfully freeze your blastocysts.
Cambridge IVF has a state-of-the-art Cryostorage facility on site. Embryos are stored at very low (-196oC) temperatures using liquid nitrogen or its vapour.
How Does the Process Work?
Before we can store your embryos, we need the consent of both the egg and sperm providers; this is a legal requirement. We will ask you to complete a series of electronic consent forms before you proceed to treatment.
There are 4 key areas we need to consider when we take legal consent to the storage of your embryos, these are:
- What should happen to the stored embryos in the event of your death or mental incapacitation? It is important that we know your wishes before we store your embryos. It may be possible to register a deceased partner as the parent of a child. All relevant implications will be discussed with you prior to treatment.
- How long do you wish to consent for your embryos to be stored for? Embryos can be stored for up to a maximum of 55 years from the date the embryos were first placed in storage. In order for storage to continue, the consent must be renewed every 10 years. The clinic will contact you at the appropriate time to let you know when renewal of consent is required. You can of course decide to freeze them for a shorter period. You can also decide at any time that you no longer want your embryos to be kept in storage - for more information on the implications of this, please see our patient information on ‘Consent to treatment’ in particular the section on ‘Withdrawing, varying and restricting consent’.
- The law does not allow us to keep your gametes or embryos in storage beyond the date you have consented to. We will be in touch with you a few months before the end of the storage period to find out what you wish us to do. It is important that you keep in touch with us, in particular that you notify us of any change of address. If the storage limit is up, and you have not consented to extending this limit, we are obliged by law to let any stored embryos perish, even if we have not been able to trace you first.
- If you wish, you can consent to the use of your embryos in research or training. In certain circumstances you may donate them for the use of other people for their treatment if you decide that you do not need the embryos for your own use anymore.
It is important that you answer these questions as clearly as you can leaving nothing open to interpretation as your wishes on these issues are required by law before we freeze your embryos.
Blastocyst Vitrification
Good quality surplus blastocysts can be frozen on day 5 following your embryo transfer. We use a process called vitrification to rapidly freeze your blastocysts which we then store in our Cryostore for you to use at any time in the future within the time period you have consented to.
On day 5 and day 6 of your cycle we will look at all the remaining embryos and decide if any of them are strong enough to be frozen. Of course this is your choice, you don’t have to have them frozen if you don’t want to, we will carry out your wishes either way. It would be beneficial to spend some time before your ET deciding what you would like to do if you do have embryos available to be vitrified.
Which embryos could we freeze?
Freezing and thawing can cause damage to the cells of an embryo. This means that only good quality embryos are suitable for freezing as poor quality embryos very rarely survive thawing. We use the vitrification technique on blastocysts to maximise the chances of survival following the freeze-thaw process.
What is the likelihood of embryos surviving the procedure?
Our data on vitrification and thawing survival rates demonstrates that we achieve survival rates of around 90%. In some cases some of the cells or all of the cells within the blastocysts may not survive. This is unpredictable and can be patient specific.
Do the surviving blastocysts resume development after thawing?
Once the blastocysts are thawed, we will closely observe the cells in the embryo to check these have not deteriorated. We will also look for signs of a process called ‘re-expansion’, which will allow us to confirm embryo viability following thaw. We will contact you to update you on the progress of the thawed embryo.
How many thawed blastocysts are required to optimise the chance success?
The chances of success with frozen thawed blastocysts are comparable to the success rates with a fresh blastocyst transfer. As blastocysts are known to survive vitrification very well, we recommend that you consider freezing any good quality blastocysts we have remaining following your embryo transfer. The number of blastocysts to thaw will be discussed with you during your treatment to optimise the chance of achieving a pregnancy but also minimise the risk of a multiple pregnancy. There are several factors to consider when deciding the number of blastocysts to transfer, such as female age, treatment history and embryo quality.
What are the risks to a child born using a frozen blastocyst?
Using frozen embryos in treatment is just as safe as using fresh embryos. At Cambridge IVF we constantly monitor our results and pass on information to the HFEA which allows high power data analysis to be carried out at a national level. This ensures that we continue to operate safely and in an informed environment.
What do we do if we want embryos frozen?
Both sperm and egg providers must give consent to freezing and storage of your blastocysts. At the time of your embryo transfer we will discuss with you the quality of any remaining embryos, so it is important we know your wishes before this point in your treatment cycle. The embryologist will let you know if freezing is recommended based on your own unique treatment cycle results. Freezing of any suitable embryos will be done on day 5, we will also freeze good quality blastocysts on day 6.
Blood samples will have been taken from both partners, to test for HIV and Hepatitis B & C. These tests are performed to allow us to store your blastocysts appropriately in a screened or viral positive storage facility as appropriate. Screening tests may be funded by the NHS or in some cases you may have to self-fund these (please refer to our website for our current pricelist). Additional tests may be performed depending on your personal circumstances and you will be informed if further testing is required during your appointment. If any of the test results return indicating an infection, we will notify you and arrange an appointment for you to see a medical practitioner.
Could anything go wrong with our Storage?
We do everything we can to maintain a high quality cryostore here at Cambridge IVF. We have a system in place that monitors the cryostore continually and will alert us immediately if there is the slightest suggestion of a problem. We use a high security storage system to reduce the theoretical risks of cross contamination between samples. Even with our exacting standards and commitment to quality, we cannot provide a guarantee that your samples may not be affected in the event of an ‘act of god’, civil disturbance, catastrophic equipment failure or any other unexpected and abnormal occurrence which may affect our service or facilities.
Clinical Results
We are very proud of our success rates at Cambridge IVF. Our results are in line with or exceed latest published national averages. We excel in cryobiology and our success rates for frozen embryo transfer are comparable with our results using fresh embryos:

Our embryologists are State Registered with the Health and Care Professions Council (HCPC) and have all attained certification with the Association of Clinical Embryologists or the Scientific Training Programme.
We have put together the team based not only on the skill of the scientists and their depth of knowledge but also their desire to make Cambridge IVF a patient focused and friendly unit which not only excels clinically but achieves this whilst maintaining a close and open relationship with our patients.
Comment on Witnessing
We are all very aware there have been IVF mix-ups in other clinics in the UK and across the world. Cambridge IVF has taken every step possible to minimise the risk of mix up occurring here and we are very proud that since we opened in 2011 we have never had a mix up event occur.
In addition to stringent checking and procedural controls being in place, we have invested in an electronic system called RI Witness which provides a further layer of transparent and auditable protection against the mixing of incorrect sperm and eggs or transfer of the incorrect embryos in your cycle. We are not saying we are likely to have made a mistake without it, this could not be further from the truth but we do believe in making our processes as safe and risk free as possible and we believe that RI Witness ensures this. We also believe it is right to inform you that such risks exist and we do everything possible to reduce them.
We hope you have found this booklet informative and interesting. We realise we may not have covered all of your questions so if you do have any other queries we are here to help so please contact us via any of the means below:
How to get in Touch
Cambridge IVF
Kefford House
Maris Lane
Trumpington
Cambridge
CB2 9LG
Follow us on:
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

