Who is this leaflet for?
The information below is designed for adults who are in a period of recovery following an acute illness of COVID-19 that affected their breathing. The aim of this leaflet is to provide practical advice to help manage breathlessness and cope with fatigue and anxiety following a hospital admission.
Managing breathlessness
What is breathlessness?
Breathlessness is a feeling of not being able to catch your breath or feeling as if you cannot get enough air into your lungs.
As COVID-19 is an infection that mainly affects the lungs it can commonly cause symptoms of breathlessness. Being in hospital following a period of illness will also cause deconditioning of your muscles, particularly the ones involves with breathing, which can also result in breathlessness.
Getting out of breath is a normal response of the body when doing something that requires physical effort. However, COVID-19 commonly causes symptoms of breathlessness at rest and when completing normal daily activities. This can be frightening and can make you feel out of control of their breathing. The symptoms of breathlessness can vary greatly from person-to-person.
Whatever the symptoms of breathlessness, there are simple techniques you can use to help improve and control your breathing.
Breathing exercises
Breathing control:
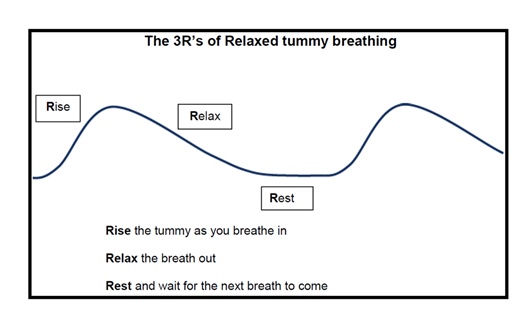
To have the most effective and efficient breaths we need to use every part of our lungs on every breath. This relies on getting good “tummy” breaths in and letting the air empty out of your lungs properly before taking the next breath in.
Sometimes people have a habit of breathing in a more inconsistent way where each breath varies (as shown below in the picture below). People that do this often use the top of their lungs and take fast, shallow breaths.

How to complete breathing control:
Breathing control may not come naturally at first. It is therefore best to practise this technique when you are not feeling breathless so that it can be used most effectively when it is needed. The picture below may help you to visualise breathing control.
- Get into a comfortable position where your body can relax, and your arms are supported.
- Put one hand on your chest and the other hand on your tummy
- Breathe in slowly through your nose focusing on a smooth breath. If you have difficulties breathing through your nose, breathe in through your mouth.
- You should feel your tummy rise and expand as you breathe in, whilst your chest should barely move.
- Breathe out gently through your nose or mouth, feeling your tummy relax down as you do.
- Gradually try to make your breaths slower and deeper. Focus on letting any tension leave your body as your breath out.
Breathing a rectangle:
This is an easy technique to control your breathing that can be adopted in any environment as there is often a rectangle to be seen e.g. a picture frame or the television. Follow a rectangle with your eyes, breathing in on the short edges and breathing out on the long edges. Try to focus on breathing control so that the breaths are coming from your tummy. Gradually try to slow the speed at which your eyes move to slow your breathing rate.

Pursed lip breathing
This technique can be useful during activities that make you feel breathless. It involves breathing in through your nose and breathing out through narrow lips, as if you were whistling. This will slow your breathing down and helps to keep your airways open so that it is easier for air to empty out of your lungs.
Paced breathing
This can help to control your breathing when you are active, such as during walking or climbing the stairs. Pace your breathing to the activity you are completing, for example, breathe in for one stair and out for one/two stairs.
Blow as you go
This technique can help to control breathing when you are exerting yourself. It can be particularly useful if there is a difficult part of an action. Focus on a breath in before making the effort and a breath out when making the effort e.g. breathing in before going up a step and breathing out whilst stepping or breathing in before standing up from a chair and breath out on rising.
Positions of ease for breathlessness
These are positions you can adopt when you are feeling breathless to help you recover. The purpose of these positions is to help to optimise the ability to get air into and out of your lungs. When using these positions, it is important that you try to let your body relax and to reduce the tension in your neck, shoulders, arms, hands, and jaw.
Resting positions
These positions may help if you are breathless at rest or if you are feeling very tired or exhausted.

Make sure you are fully over on your side. Resting your upper arm on a pillow may also help.

Relax down onto the pillows as much as possible. Having your legs apart may also help.
Positions to ease breathlessness after activity
These positions can help relax your breathing following exertion both at home and when out and about. No one position suits everyone, and you should experiment with different positions to help determine which ones work best for you. Leaning forward can help to improve the movement of your diaphragm and resting your arms in front of you, on your head/back or above your head can all be helpful to relax your breathing.
Sitting
Sitting down can be particularly helpful to ease breathlessness as it uses less energy than standing.


Standing





Walking unaided
When walking without an aid, the following techniques may help you relax your breathing by supporting your arms:
- Place your hands on your hips
- Place your hands in your pockets
- Stick your thumbs through your belt loops
- If carrying a shoulder bag, rest your arm on your bag.
Walking with aids
Some people may find that pushing a supermarket trolley helps then to walk further and feel less breathless. This is because the trolley allows you to adopt the ‘lean forward position of ease’ whilst walking.
A walking frame works in a similar way and also provides a portable leaning post when you wish to stop and rest. A walking stick can also provide a portable leaning post. When walking outdoors, people often prefer to use a three- or four-wheeled walker. Some walkers have a seat so you can sit to rest, others may have a handy storage compartment for bags.

Prone lying
Prone lying or ‘proning’ basically means to lie on your front. This is a really good position to help with your breathing and to get oxygen into your blood supply from your lungs. It helps by preventing the air-filled sacs at the back of your lungs from closing down and those at the front of your lungs from being over-inflated, both of which can prevent the movement of oxygen from your lungs to the blood. It also helps by preventing your lungs and diaphragm from being squashed by heavy organs such as your heart and abdominal content. These changes can often happen when you have been lying on your back for a long period of time. Turning onto your front can help to reverse them.
The pictures below demonstrate different positions you can use to achieve prone lying. You should try to lay in one these positions for 1-2 hours a day. If you become uncomfortable in one position, try swapping to another. For further advice on prone positioning, please speak to a physiotherapist.

Do not try these positions if:
- You are unable to get yourself in and out of these positions on your own
- Your breathing rate is higher than 35 breaths a minute
- If you have a low blood pressure or are known to have cardiac arrhythmias
- If you have a spine or thoracic injury or have had recent abdominal surgery
Seek advice from a healthcare profession before trying these positions if you:
- Have a facial injury
- Have a long-standing neurological issue (such as seizures)
- Have a BMI over >40
- Are in the 2nd or 3rd trimester of pregnancy
- Have pressure sores / ulcers

Position 1: lie flat on your tummy, turn your head to the side and tuck both arms under your chest/shoulders. Try to ensure your feet are off the end of the bed. You can stack pillows under your shins to support your feet off the bed if needed.

Position 2: lie on your tummy with a pillow under one leg to support your pelvis. Place both hands flat above your head, in whichever position is comfortable for you. Try to ensure your foot is off the edge of the bed.

Position 3: lie on your side with a pillow between your knees and a pillow under your shoulder/trunk so you can rest your tummy forwards onto the pillow. Try to ensure your foot is off the end of the bed.

Position 4: lie on your front with a pillow under your tummy, turn your head to the side and place your hands flat above your head in whichever position is comfortable for you. Try to ensure your feet are off the end of the bed. You can stack pillows under your shins to support your feet off the bed if needed.
Managing fatigue and energy conservation
What is fatigue?
Fatigue is a deep feeling of tiredness that rarely goes away and is a common symptom during recovery from COVID-19. It can affect people in different ways and can be very debilitating to everyday life. It can make daily tasks such as washing and dressing difficult and aggravate symptoms of breathlessness.
There are several ways that you can adapt your lifestyle to help conserve energy and manage the symptoms of fatigue and breathlessness. Adopting a few of these habits can make a big difference to your everyday life.
Time management
It is important to plan your time appropriately to avoid overexerting yourself. It may be useful to keep a fatigue diary so you can track your fatigue at different parts of the day, particularly following activities. By knowing which periods of the day you have more or less energy, and what activities you find particularly tiring, you can plan your day more appropriately.
Consider making a timetable for the day or week to allow you to spread out strenuous tasks and incorporate periods of rest into the day. Prioritise which tasks need to be done that day and which could be left for another day. If you have appointments try to schedule the times that best suit you and allow plenty of time to get there. This may be useful to do in conjunction with your fatigue diary.
Give yourself ample time to complete a task and avoid rushing which may aggravate symptoms of breathlessness and cause anxiety. Make sure periods of seated or lying rest are factored into every day, particularly after strenuous activities.
Making tasks more manageable
Try to find ways to break down activities into different sections that can be spread out. For example, when cleaning the kitchen, you may take the bins out one day and sweep the floor the next.
Consider how you can make tasks that are essential easier so that you have more energy for tasks that you want to do. For example, when showering use a toweling dressing gown to reduce the effort of drying yourself and choose clothing and shoes that are easy to slip on and off.
Try to organise your environment to make tasks easier for you. Keep items that you frequently use in an easily accessible place and ensure you bring essential items downstairs with you in the morning to avoid multiple trips up the stairs. Consider rearranging your cupboards to ensure popular items are at an easy height for you to access to avoid overhead reaching, bending too low or heavily lifting. Try to avoid long periods of standing throughout the day. For example, consider sitting at the kitchen table or on a perching stool to prepare meals.
Pacing
It is important to recognise your limitations and work within them. Take time when doing activities and stop if you begin to feel tired. Use your level of breathlessness to help guide you when to slow down or stop. Avoid overexerting yourself in one activity, even if you are feeling good, as it may have a knock-on effect later in the day or week which may take longer to recover from.
Sleep
It is important to make sure you get enough sleep. Try to avoid drinking caffeine and alcohol prior to going to bed and avoid going to bed too late. Limit your exposure to bright light, loud noises, and electronic devices when you are preparing to sleep. You could consider using apps that provide guided mediation and promote relaxation if you have problems falling asleep.
Put your needs first
Avoid overcommitting yourself to activities or social events. Where possible, delegate tasks such as household cleaning or washing of clothes to other members of the family. Accept support from family or neighbours with tasks such as food shopping. Investigate services in the community that can support you with tasks such as shopping, cleaning, and gardening. This will allow you to conserve energy for activities that are important to you.
Stress and anxiety management
The experience of being admitted to hospital with COVID-19, and particularly intensive care, can cause a lot of stress and anxiety. As can living with the symptoms of breathlessness.
The information below provides some easy measures you can adopt to help reduce stress and anxiety.
What to do in the moment:
1) If you start to feel anxious, stop what you are doing.
2) Try to break the cycle by removing yourself from the situation and going somewhere quiet.
3) Focus on breathing techniques to try to help calm yourself.
4) Be aware of any muscles that you are tensing and allow them to relax.
5) Try talking to yourself to help manage negative thoughts
If you cannot take yourself away from the situation try saying or imagining:
- 5 things you can see right now
- 4 things you can hear right now
- 3 things you can touch right now, reach out and touch them
- 2 things you can smell or like to smell
- 1 slow, deep breath. Focus on your breathing. Only once your breathing has relaxed should you shift your focus.
Breathing techniques
When people feel stressed or anxious it cause them to breathe rapidly and often aggravate symptoms of breathlessness. Breathing techniques, such as breathing control and rectangle breathing, can be a good way of managing symptoms of anxiety when they arise.
Another very quick and effective calming technique is colour breathing. As you breathe in imagine the colour blue as calm and as your breath out image the colour red as tension leaving your body.
Some people also find using a handheld fan in front of their face can help to ease symptoms. For more information on breathing techniques section.
Have a routine or schedule
Having a routine for your daily activities can be a great way of organising tasks and avoiding being overwhelmed. It also means you can incorporate periods of rest and relaxation into your day. Consider making a to-do list to help you prioritise tasks and to avoid anxieties associated with trying to remember what needs completing. This can also be a really good way of keeping a visual record of what you have achieved.
Setting goals
Set yourself goals of what you want to achieve. Be realistic and flexible in achieving them and do not give yourself unrealistic deadlines.
Talk about it
Talk with family and friends and make them aware of how you are feeling and the signs and causes of your stress. Together come up with some ideas of how to manage your symptoms when they arise so they know how best to support you.
Stay in contact
Recovering from illness both in hospital and at home during social distancing can cause feelings of loneliness. Make sure you stay connected with people via the telephone or through emails or phone messages if you find talking aggravates your breathlessness.
Relaxation techniques
Relation is an important part of stress management and it is essential to give yourself time in each day for rest and relaxation. Relaxation techniques can be an effective way of reducing your anxiety. There are many guided relaxation techniques available online to help you to relax. Why not try this one?
- Get yourself in a comfortable position in a quiet room, such as in a chair or lying on your bed
- Close your eyes and focus on taking a slow, deep breath in and then out
- Imagine you are in an environment you find calming such as lying on a beach or sitting by a lake. Imagine the sounds and sensations you would experience there, like the sound of waves gently crashing on the shore or the feel of a light breeze on your face.
- Starting with your face and working down to your toes, slowly tense your muscles. Hold them for a few seconds, and then allow them to relax. Feel the tension leave your body as you relax.
- This technique should take 5-10min
Meditation and mindfulness:
Like relaxation, mediation and mindfulness exercises can be very calming techniques that help to refocus your mind. Many apps and YouTube videos online provide guided meditation that you can do from a quiet room at home.
Reading and audiobooks
Reading and audiobooks can be a great way to switch off and divert your attention from negative thoughts.
Music and radio
Listening to music, radio or podcasts can help you to switch off. Listening to your favourite music or a funny or relaxing podcast can help to provoke positive emotions.
Smells
Smelling is an immensely powerful sense; it can be very calming and help you feel present in the moment. Find a smell that you find relaxing or brings back happy memories and use it when you are feeling anxious. For example, fresh flowers, dried lavender, or scented candles.
Creative hobbies
Hobbies such as drawing, colouring, knitting or puzzles can be very therapeutic and a good way of distracting your mind from negative thoughts. Why not try taking up something new?
Keep active
Exercise leads to positive changes to physical and mental wellbeing. It can help to relief stress in a positive way and can help to reduce breathlessness by improving physical fitness.
Exercising outside of your house, whether it be walking around your garden or a park, can be a really good way of getting some fresh air and a change of scenery which can also help your mental wellbeing. Maybe try something new such as Tai Chi or Yoga which help you to focus on your breathing whilst you exercise.
For ideas of appropriate exercises for you, speak to your physiotherapist.
Breathlessness and exercise
Why should you stay active?
It is important that you stay active as this will help to keep your muscles strong and improve your breathlessness. Often when people experience breathlessness, they may try to limit the amount of exertion they do to avoid being short of breath. When you stop being active the vicious cycle of inactivity occurs. This can lead to the loss of physical fitness, weaker muscles, and greater levels of breathlessness.

How to stay active
Avoid long periods of sitting or lying and try to increase the number of steps you take a day. Smartphones and pedometers can be good tools to help you set daily step targets.
It is important to do a mixture of aerobic exercises, designed to get you out of breath by working your heart and your lungs, and resistance exercises to build your muscle strength and endurance. Research suggests adults should complete 150 minutes a week of moderate intensity aerobic exercise - about 20 minutes a day. This may include activities such as walking, swimming, or gardening. Adults should also do resistance exercises several times a week to build muscle strength.
Use the breathing techniques to help you control your breathing during exercising and positions of ease to help you recover afterwards. By completing regular physical activity, it will help you to feel less out of breath doing everyday activities and improve your energy levels.
When exercising, make sure you pace yourself, so you do not get too tired too quickly. It is important to keep your breathlessness in mind and you can use the BORG scale below to ensure you work within the right parameters for you. Instead of working to a set number of exercises, work until you feel breathless, rest, and then repeat. During activities you should still feel like you can talk if needed. Speak to your physiotherapist to determine exercises which are appropriate for you.
Measurements of breathlessness
The tool below can be used to help you rate your breathlessness at rest and when completing activities. This can help you to tailor your exercises to the correct intensity and to help you to monitor your fatigue and breathlessness levels during the day.
The modified BORG dyspnoea scale
The BORG Scale allows you to rate the difficulty of your breathing starting at number 0 where your breathing is causing you no difficulty at all and progressing through to number 10 where your breathing difficulty is maximal. When completing exercises, someone in previously good health should aim for a score of 6-7. Someone with a chronic health condition which normally affects their breathing should aim for a score of 3-4.
| 0 | Nothing at all |
|---|---|
| 0.5 | Very, very slight (just noticeable) |
| 1 | Very slight |
| 2 | Slight |
| 3 | Moderate |
| 4 | Somewhat severe |
| 5 | Severe |
| 6 | |
| 7 | Very Severe |
| 8 | |
| 9 | Very, very severe (almost maximal) |
| 10 | Maximal |
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

