Key messages for patients
- Please read this information carefully. You and your health professional will sign this to document your consent.
- Please bring with you all of your medications and its packaging (including inhalers, injections, creams, eye drops, patches, insulin and herbal remedies).
- If you are taking warfarin tablets, please bring with you the result of an INR test performed within the week before the planned injection.
- Please call the clinic sisters on telephone number 01223 217778 if you have any questions or concerns about this procedure or your appointment.
After the procedure a copy of your consent will be scanned in to your clinical record system. You will be advised to take this information leaflet home with you.
Important things you need to know
Patient choice is an important part of your care. You have the right to change your mind at any time, even after you have given consent and the procedure has started (as long as it is safe and practical to do so).
We are unable to guarantee that a particular person will perform the procedure. However the person undertaking the procedure will have the relevant experience.
All information we hold about you is stored according to the Data Protection Act 1998.
Blepharospasm
Blepharospasm is characterized by abnormal contraction of the muscles around the eye. This can range from a mild eyelid twitch to involuntary blinking or even full closure of the eyelids. It usually affects both eyes, but can sometimes involve just one.
The exact cause is unknown, but it is often attributed to a loss of control of the natural blink reflex. Blepharospasm can follow a particular pattern and might be worse at different times of day. It can be triggered by things such as bright light, stress, or fatigue.
It often lasts only a few minutes, but in severe cases can last much longer, resulting in difficulty in performing activities of daily life due to difficulty keeping the eyes open consistently.
What is Botulinum toxin?
Botulinum toxin is a drug which causes muscles to relax. It is naturally produced by a bacterium called Clostridium Botulinum. More commonly known by the brand name “Botox®”, it is now manufactured for use as a medical treatment for a number of neuromuscular conditions.
How does Botulinum toxin work?
Nerves connected to muscles cause them to contract by releasing a chemical signal called Acetylcholine. Sometimes this signalling can become overactive, causing involuntary muscular movements such as eyelid spasms and facial tics. In rare cases, prolonged contraction and cramping can result in chronic, debilitating pain. Botulinum toxin temporarily stops nerves from releasing Acetylcholine. Without this neurotransmitter, muscles do not contract and remain in a relaxed state. (Fig 1).
The toxin weakens some of the muscles that close the eyes or cause spasm. This decreases the frequency of blinking and the uncontrollable spasm.

Botulinum toxin injections are also used for Hemifacial spasm treatment, a similar condition to blepharospasm. More commonly occurring on just one side of the face, hemifacial spasm involves more muscles than just those around the eye. The cheek and corner of the mouth on the same side contract involuntarily, resulting in what is commonly referred to as a “facial tic.”
Hemifacial spasm is better understood than blepharospasm: some patients are found to have a blood vessel that sits in close proximity to the facial nerve (Fig 2), intermittently touching it and causing abnormal activation. Following facial paralysis for other causes (such as Bell’s Palsy), aberrant recovery of the facial nerve can result in paradoxical hyperactivation.

Intended benefits of botulinum toxin injection for blepharospasm
As explained above Botulinum toxin injection works by blocking the release of acetylcholine at the neuromuscular junction, the toxin weakens some of the muscles that close the eyes or cause spasm. This decreases the frequency of blinking and the uncontrollable spasm.
The injections start to work after 24 to 72 hours, having maximum effect by 2 to 3 weeks. The effect of the injections last for 8 to 12 weeks and repeated injections are necessary for continued relief and consistent symptom relief can be achieved with about four to five injections per year. Regular treatment can result in a more prolonged effect, requiring fewer injections over longer periods of time. Very rarely, the opposite can also occur: resistance to the treatment can also develop, leading to more frequent injections in a shorter period of time.
Every case is different—even the sites and strength of the treatment administered to you at each visit may vary. One side of your face may respond differently to the other. Many factors interact and play a role in the efficacy of the treatment. Your doctor and the nurse will be working with you to tailor the appropriate regimen for your symptoms.
Who will perform your procedure?
The initial set of injections will be given by an ophthalmologist. Once a satisfactory response to the injections is confirmed, subsequent injections will be given by a trained ophthalmic nurse specialist.
The injector (doctor/nurse specialist ) must be trained in consent and be deemed competent by the supervising consultant before independent practice takes place. Written consent for the procedure must be taken prior to the first injection taking place in line with the Trust’s Consent policy for examination, treatment and post mortem. You must have been given a copy of the relevant patient information leaflet prior to signing the consent form.
A copy of the consent form must be scanned in to your clinical record you’re your first treatment is completed. Consent is valid until the treatment is needed. It is the injecting nurse’s responsibility to ensure the consent is obtained and scanned in to patient record.
Before your procedure
You will meet an ophthalmologist (eye doctor) at your oculoplastic clinic appointment. Your doctor will discuss the planned procedure and decide on the site and number of injections required. At this clinic, we will ask for details of your medical history and carry out any necessary clinical examinations and investigations. Please ask us any questions about the procedure, and feel free to discuss any concerns you might have at any time.
We will ask if you take any tablets or use any other types of medication either prescribed by a doctor or bought over the counter in a pharmacy. Please bring all your medications and any packaging (if available) with you. Please tell us if you take Warfarin, Aspirin, Rivaroxaban, Dabigatran, Apixaban, Edoxaban or Clopidogrel, Ticagrelor or blood thinning medication you might not be suitable for treatment.
This procedure does not involve the use of an anaesthetic before the injections. You therefore, do not need to fast before your botulinum toxin injections.
Botulinum toxin injection is usually performed as a minor procedure in the outpatients department.
Botulinum toxin injection is not a suitable treatment if you are pregnant or ‘trying’ for a baby.
If, to your knowledge, the answer to any of the following is yes, it is important that you tell us. Have you ever:
- received Human Growth Hormone?
- had brain surgery prior to 1992?
- or has anyone in your family been diagnosed with CJD?
A positive answer will not stop any treatment, it will however allow us to plan your treatment so as to minimise any risks.
During the procedure
You will be seated in a comfortable reclining chair. Depending on the severity of the eyelid spasm, small doses of botulinum toxin are injected just under the skin at two to six different sites around the eyelids. The exact dose and the site of injection may be varied depending on your response to previous treatments.
After three to four days, the injections cause temporary weakness in the muscles of the lids. This relieves the symptoms of blepharospasm for approximately two to three months.

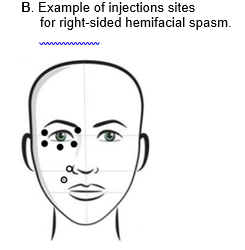
Figure 3. UK Ophthalmology Alliance: Clinical practice pack for non-medical practitioners: Botulinum toxin injection for blepharospasm and hemifacial spasm
After the procedure
Immediately following the treatment, you may temporarily experience mild pain, redness, or swelling at the injection sites. There may be minimal bleeding. These symptoms are common, and under no circumstances must you apply pressure or rub the injection site. Doing so may cause the toxin to migrate to the surrounding tissues, causing unwanted effects. If you notice some bleeding, take some soft tissue or cotton ball and gently dab the area; the bleeding should stop in a few minutes. Rarely does the pain from Botulinum toxin require an oral pain reliever, but you may if you feel the need to do so.





Significant, unavoidable or frequently occurring risks of this procedure
Following this procedure, the majority of individuals with eyelid spasm experience relief from their symptoms. However, occasionally, some bruising develops around one or more of the injection sites. If some bruising is noticed in the first few hours after injection, applying pressure to the area with a cold compress (such as a bag of frozen peas) can reduce the swelling.
Sometimes, the muscles of the eyelids can become weaker than expected following the injection and can cause drooping of the eyelids. Occasionally you will experience ‘double vision’. Because the effects of the toxin injection are temporary, this excessive weakness will resolve with time, but might last two to three months. If you experience these problems, please contact the eye clinic for advice and be sure to inform the ophthalmologist and nurse at your next appointment, so that the dose and site of the injection can be modified in future.
Alternative procedures that are available
Botulinun toxin injection is the best available for the treatment of eyelid spasm.
Rarely surgery may be required for genuine treatment failure.
Information and support

You might be given some additional patient information before or after the procedure, for example: leaflets that explain what to do after the procedure and what problems to look out for. If you have any questions or anxieties, please feel free to ask a member of staff.
Further information about eyelid spasm is available from The Dystonia Society.
Tel: 02077933651 or visit the Dystonia website (opens in a new tab).
Document details
Approved
14 Jan 2025
Version number
7
Document ID
1846
Other formats
Help accessing this information in other formats is available. You can find out more about this service on our patient information help page.
Service / Department
Ophthalmology
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

