Introduction
This leaflet is for caregivers of children who may require an antegrade continence enema (ACE). It provides information on the ACE in children, including information on the operation itself, alternative treatments and care given before and after surgery. The leaflet also gives advice and information about caring for your child’s ACE at home to supplement the advice given by your doctors and nurse specialists. Please keep this leaflet for reference as it contains information about continuing care and problem-solving at home.
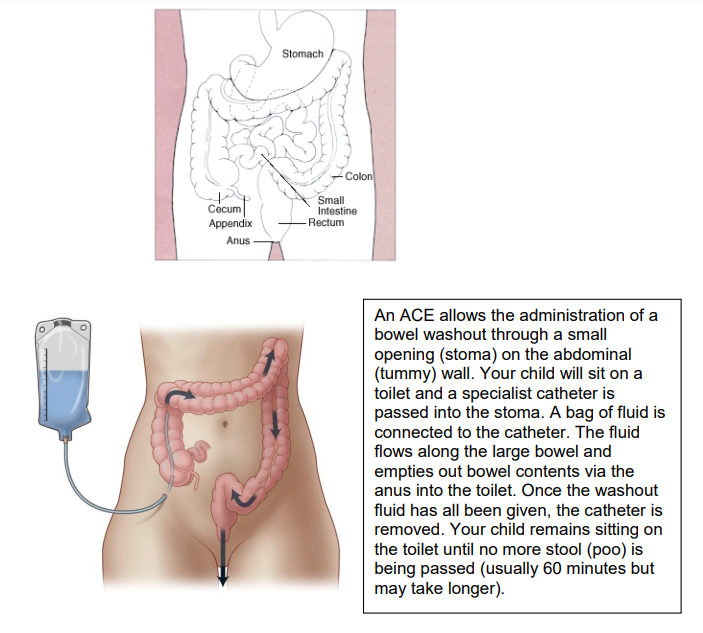
What is an antegrade continence enema (ACE)?
An antegrade continence enema, commonly referred to as an ACE (but also referred to as a MACE), is a method by which the bowel can be emptied to help in the management of constipation and faecal soiling (that is, the leakage of faeces or poo other than during a bowel movement.) An ACE may be recommended when alternative methods fail (see section of alternatives below).
During the surgical formation of an ACE, the appendix (or a small section of the child’s small bowel) is used to form a channel (tube) between part of the child’s large intestine (bowel) called the caecum, and the child’s skin.
The aim in most cases is for children to be independent in administering their washouts but this takes some time and planning to achieve and depends on the child’s age and mobility.
Why might my child require ACE formation?
Constipation and soiling may occur in children for many reasons:
- Abnormalities which are present at birth (called ‘congenital abnormalities) which affect the anus (back passage) or rectum (part of the large bowel where stool is stored before being passed from the body).
- Congenital spinal abnormalities such as spina bifida.
- Spinal abnormalities which were not present at birth (called acquired abnormalities) following severe trauma.
- Idiopathic constipation; this is the term given to children who experience constipation and / or soiling without a known physical cause.
In most cases, constipation and soiling for any of the above reasons can be managed with alternative methods to the ACE (see section on alternatives below). Formation of an ACE is therefore reserved only for children for whom all other methods of treating constipation and soiling have been trialed over many months, with full commitment from the child and family, and yet symptoms have not improved.
What are the benefits of having an ACE procedure?
- Allows stool to be cleared when other methods have been trialled and failed.
- More discreet than other types of surgical stoma; no bag is needed on the skin to collect faeces and, after the initial four to six weeks, no catheter is left inside the body.
- Allows children, particularly those with dexterity problems, to be independent with their toileting.
What are the complications, risks or problems related to an ACE?
Risks, complications and problems may occur at the time of surgery (rare), in the initial weeks after surgery when the indwelling catheter is in place and in the long term (more common).
Complications at the time of, and immediately after, surgery are rare but include:
- Bleeding
- Perforation of the bowel
- If the blood supply to the bowel used to form the ACE channel is impaired the tissue can die, requiring further surgery to re-fashion it.
Complications / problems whilst indwelling ACE catheters are in place are not uncommon and include:
- Bleeding at the site
- Wound infection
- Leakage of faeces around the ACE catheter
- The catheter placed at the time of surgery may fall out, possibly requiring a further operation to replace it or re-fashion the channel.
- Blockage of the catheter
- Migration of the catheter further into the bowel
- Painful washouts caused by bowel spasm as washout fluid is administered. The bowel preparation plan is designed to minimise this pain but children may still experience sensations they regard as unpleasant or painful as they get used to the feeling of the washouts. In severe cases children can feel nauseous, vomit or faint.
Complications / problems in the longer term:
- Some children find that the ACE irrigations do not work for them, for example, due to:
- ongoing constipation,
- ongoing or worsened soiling,
- irrigation fluid inserted via the ACE is not evacuated.
- Tract stenosis: this means that the ACE channel becomes narrow and so the intermittent catheter becomes difficult, or even impossible, to insert.
- Creation of a false passage: this means that a passage outside the channel is formed, usually as a result of tract stenosis or difficulty with catheterisation. If a false passage is created more surgery will be required and more time with an indwelling catheter in place will be needed.
- Adhesions (rare): this is scar tissue formation which can occur after any abdominal operation. It is a small but lifelong risk which may result in an obstruction (blockage) of the bowel. Symptoms of an adhesion obstruction include cramping abdominal pain and green (bile) vomit.
- Ongoing pain during washouts despite dose and speed of administration of washouts being adjusted.
- Longer term ineffectiveness: Findings from longer term research studies are informing us that, even when children have initially had a good response to their ACE and achieved cleanliness, many will, over time, find their washouts become gradually less effective with exacerbation of constipation and / or soiling again.
What are the alternatives?
Alternative therapies for the management of constipation and soiling can be grouped as follows:
- Oral laxative medication - There is a wide range of oral laxative medications available, some of which help to soften stool and others which help the bowel to push stool along. Children often benefit from a combination of laxatives. It is important that sufficient time is given to trying different laxative combinations and assessing their effectiveness.
- Rectal laxative medication - Laxatives can be given rectally (directly into the back passage) in the form of suppositories or enemas. It is not uncommon for children to benefit from a combination of oral and rectal laxative medication.
- Transanal irrigation - Transanal irrigation involves administering fluid (sodium chloride or water depending on the child’s age) into the child’s rectum, via the anus, and then allowing the fluid to be expelled along with the stool (poo). There are a number of different devices available for transanal irrigation in children. Transanal irrigation can be taught by the nurse specialist team, is undertaken at home and does not require any surgery. Whilst it can often take a few months to identify the most appropriate transanal regimen for the child, the ever increasing range of devices has meant that even young children have been able to successfully participate in their own transanal irrigation.
- Formation of a colostomy stoma - A colostomy formation is an operation to bring a section of large bowel (colon) out onto the surface of the skin. A bag is placed over the opening of the bowel to collect the stool. Colostomy formation is most commonly performed in the neonatal period as a result of a congenital problem being diagnosed (for example, ano-rectal malformation) but it is exceptionally rare for a colostomy to be formed for the purpose of easing constipation / soiling in the older child.
Before admission to hospital
Deciding to proceed with formation of an ACE
The decision to proceed with formation of an ACE is a significant one. Therefore you and your child will meet with a team of experienced specialists. They will assess your child in relation to whether ACE washouts are likely to be helpful in the management of their constipation / soiling and also, importantly, they will assess whether your child is psychologically ready for ACE washouts. It is not uncommon that surgery to form an ACE is delayed to allow the child time to be adequately prepared for their ACE washout regimen. Whilst this may feel frustrating, it is essential that an ACE is not formed until a child is psychologically ready in order to ensure willingness to use the ACE after surgery.
You and your child will meet with specialists including a paediatric surgeon, clinical nurse specialist and play therapist and may also meet a children’s psychologist and / or children’s dietician.
Once a decision is made that ACE washouts are necessary and that your child is adequately prepared for receiving ACE washouts, referral will be made to a local children’s community nurse. Your child’s school will be informed about ACE – this is usually via the community nursing team. Although ACE washouts will not be performed at school or impact on the school day, nonetheless it is important that the school team are aware of what an ACE is and the treatment your child is receiving.
Purchasing suitable painkillers
It is important that you purchase some children’s pain killers such as paracetamol (for example Calpol) and ibuprofen before admission to hospital so that you have these available at home after discharge.
If your child becomes unwell
If your child has a cold, cough or illness such as chicken pox, the operation will need to be postponed to avoid complications. Please telephone us to discuss this with us (the telephone number is at the end of this leaflet).
Preoperative assessment and blood tests before the operation
You will be asked to complete a health screening questionnaire when your child is added to the waiting list; this will be completed over the telephone.
Blood tests will be required, and these are taken within four weeks of the operation date.
What is ‘bowel prep’ and will my child need this?
Bowel preparation (commonly referred to as bowel prep) involves the clearing of stool from the colon (large bowel) to prepare it for surgery and reduce risks such as infection and, in the case of ACE surgery, to prepare it for the commencement of ACE washouts. Initial ACE washouts can be painful if the colon is full of stool (poo) so, by emptying it before the operation, children are more likely to have an uneventful first washout which improves their willingness to continue.
Every child that requires bowel prep will have an individualised care plan made for them and you will be given a copy of this before admission to hospital. Bowel prep is likely to involve the following:
- An intake of a low residue diet for a few days at home before surgery. You will be provided with a list of suggested foods and those to avoid. Once children are admitted to hospital, the intake of foods (apart from clear ice lollies, clear soups, clear jelly and boiled sweets) is stopped.
- Children can drink normally until admission and then will only permitted to drink clear drinks (water or sugared squash) from the time of admission.
- Children will receive oral laxatives designed to clear the bowel of faeces. Usually children receive higher doses of their usual laxative and the initial doses are given at home. You will be advised of any changes to their normal medication.
- To clear the bowel of faeces, some children will also require bowel washouts via the rectum. Bowel washouts are carried out on the ward by a nurse and you can be present during this. Bowel washouts are not painful; the nurse will ensure that your child is kept warm and as comfortable as possible. Children lie on their left side so you will be able to position yourself so your child can see you and have a story read to them for example. Bowel washouts involve passing a small tube a short way into the back passage. A syringe is attached to the other end of the tube and a small amount of warmed salty water is then poured into the syringe. The water flows by gravity down the tube and into the child’s bowel. Once the water is in the bowel the syringe and tube are lowered to enable the water, now containing faeces, to run back out and be collected in a container. This process is repeated several times. The number of washouts required will be stated in your child’s individualised care plan, although the amount does also depend on the result of each washout (how much faeces is cleared). As the aim of the bowel preparation treatment is for the bowel to be completely clear of stool before the operation, it is important that when the last washout is performed the fluid that runs back out of the stoma/rectum is clear.
What will happen when my child is admitted to hospital?
You will be asked to bring your child to one of our children’s wards one to two days before the day of surgery to:
- complete their bowel preparation,
- have their blood sugar levels monitored,
- have their hydration level monitored.
- If not required earlier, most children will have a cannula (drip) inserted on the afternoon prior to surgery and intravenous fluids started to ensure your child is well hydrated before their operation.
You will be asked to sign a consent form. On the day of surgery one parent is welcome to accompany their child when they go to the anaesthetic room to go to sleep for the operation and can also be present in the recovery area when they wake.
What happens during the operation?
The operation is performed under general anaesthesia and, in most cases, can be performed using a laparoscopic (keyhole) technique. The operation takes approximately two to three hours.
Where the appendix is available and of sufficient length, the appendix is used to form the ACE channel. If your child’s appendix has previously been removed or is found to be too short, the surgeon will create the ACE from a section of small bowel.
The surgeon will remove or reposition the appendix (or section of small bowel) from its normal position, whilst maintaining its blood supply. The end of the appendix is opened up to form a channel (tube) with one end attached to the large bowel and the other end connected to the surface of the skin on the child’s lower right side (usually just beneath the level of their waistband).
The opening at skin level is called a stoma. A catheter will be passed into the stoma down the ACE channel and the balloon of the catheter inflated within the bowel. This catheter is referred to as an ‘indwelling catheter’ and it remains in place for four to six weeks whilst the wound heals.
What will happen after the operation?
You will be contacted via your mobile phone when your child is waking in the recovery area, so that you can be with them again. After a period of monitoring in the recovery area your child will be taken back to the ward or, if they require closer monitoring due to any underlying condition, to our children’s high dependency unit.
Your child will return from their operation with:
- a catheter via the ACE– this will stay in place for approximately four to six weeks
- a cannula (drip) through which fluids, painkillers and antibiotics can be administered until your child is taking drinks and medicine by mouth again (usually one to two days)
- Children who have had their ACE channel formed from small bowel may have a naso-gastric tube (NG tube) after their operation. This is a tube which passes into the stomach via the nose to help drain the stomach and prevent vomiting while the bowel recovers. The tube is removed once children can manage fluids by mouth again.
The nursing team will measure your child’s urine output carefully and will need to know the volume of any drinks taken.
Once your child has eaten a normal diet for a full day, an oil (usually Arachis oil unless your child has a peanut allergy) will be administered through your child’s ACE catheter. This is to soften the stool, lubricate the bowel and therefore prevent spasm during the first washout.
You will be taught how to look after your child’s ACE site at home including cleaning, how to perform ACE washouts, problem solving and reasons to call for advice.
How long will my child stay in hospital for and can I stay with them?
The time from admission to discharge is usually seven to ten days in length. This includes the time for bowel preparation, surgery and recovery. One parent can stay over with their child.
At the time of discharge your child’s nurse specialist will arrange a date for your child to be reviewed, have their ACE catheter removed and be taught to perform intermittent catheterisation via their ACE.
What fluid, and how much fluid, is used for the ACE washout and why?
The volume of fluid used for an ACE washout is calculated based on your child’s weight and is usually 10 to 20ml per kilogram of your child’s weight. For example, a child weighing 25kgs will require 250 to 500ml of fluid. Research findings inform us that when 0.9% sodium chloride is used as the washout fluid, the least changes are seen in the child’s blood electrolyte (salt) levels and the least side effects are seen.
In adults, tap water is more commonly used as a washout fluid and, in older children (aged over 10 years), short term use of tap water is acceptable for example when travelling on holiday. However, tap water used must also be suitable for drinking.
Sometimes, when washouts become ineffective, it is necessary for a laxative to be added to the washout fluid. Your nurse specialist and doctors will advise if this is necessary and how to administer this. Children who need some types of laxative to be added to their sodium chloride washout fluid require annual blood tests (more frequently if the child has altered kidney function).
How often are ACE washouts performed?
Most children start with daily washouts but once they have achieved effective, pain free washouts without soiling, the frequency may be gradually reduced until your child receives their washouts on alternate days.
It is important to perform the ACE washouts at the same time of day for example consistently on waking, or consistently on getting home from school or consistently before bed as this helps the body to get into a routine and so washouts become more effective.
Will my child still need to take oral laxatives?
Whether or not your child will still need to take oral laxatives will be assessed over time by your child’s doctor and nurse specialist.
Discharge advice - How do I look after my child at home whilst they have an indwelling ACE catheter?
Follow the procedure for your child’s ACE washouts and document carefully the regimen used, time of washout, result and any leakage between washouts. Your nurse specialist will telephone you to discuss progress in these areas and use this information to fine-tune your child’s regimen.
Daily cleaning of the ACE site
- Before your child is discharged you will be shown how to clean and dry and change dressings at your child’s ACE site. Some leakage is to be expected in the days and weeks following surgery and, because of this, and because your child will have a catheter in place, it is important to keep the area clean to prevent infection.
Emergency care box
- Before your child is discharged you will be provided with an ‘emergency care box’ which will contain items to be used in the unlikely event of the catheter becoming displaced. It is essential that this care box is kept with your child at all times.
What is an ACE stopper?
An ACE stopper is a small, plastic plug which has the appearance of a small plastic, blunt ended drawing pin.

An ACE stopper is used to prevent tract stenosis (narrowing) after the indwelling catheter is removed from the ACE tract. After a few months, children are encouraged to wean off using an ACE stopper as their use can result in increased faecal leakage onto the skin. If an ACE stopper is not being used, a catheter must be passed into the ACE tract twice daily to prevent stenosis of the tract (after a period of time some children can pass a catheter once daily only).
Other frequently asked questions:
Troubleshooting
Indwelling ACE catheter has fallen out
Action needed:
- Don’t panic! Collect your child’s emergency care box (containing spare catheter, lubricating jelly, catheter valve, tape).
- Apply lubricating jelly to the tip of the catheter and then pass the catheter down the ACE stoma until half of the catheter length has been inserted. Tape in position. Attach the new catheter valve. Where the same size catheter cannot be inserted, use a catheter one size smaller.
- Call your care team and do not use the catheter until an X-ray has been taken to confirm its position and the balloon has been inflated.
Catheter valve on the indwelling catheter is broken
Action needed:
- Wash hands
- Gently remove the broken catheter valve
- Push the new catheter valve tightly in place
- Check that the tap is in the ‘off’ position.
Sodium chloride will not run down the irrigation bag and into the ACE channel
Action needed:
- A piece of stool (poo) has probably blocked the tip of the catheter.
- Draw up 50ml of sodium chloride into a 50ml catheter tipped
- syringe.
- Gently inject this to clear the blockage.
Discharge is observed from the ACE stoma
Action needed:
- It is normal to get discharge from the ACE stoma whilst a catheter is continually in situ. The discharge may be clear / coloured.
- It is important to clean an ACE site daily.
- If the site has pus discharging, then antibiotics are required; contact your nurse specialist or GP.
Excretion from anus is running clear before all the sodium chloride has been given
Discuss with nurse specialist either:
- decreasing the volume of sodium chloride
or
- decreasing the frequency of the washout.
At the end of the washout the output is not running clear
Action needed:
- Check weight of your child to ensure that the volume of sodium chloride being administered is 20ml per kg of body weight.
- Liaise with your nurse specialist. If your child’s weight has increased, they may require a larger dose or your child may require a laxative to be added to the washout regimen.
Washout given but no result (that is no excretion from anus) - ‘failed washout’
- Observe for leakage overnight.
- If fluid has not been passed by the morning, contact your nurse specialist.
Child has leakage / continued soiling between washouts
Action needed:
- Increase time the child sits on the toilet post washout.
- Liaise with the nurse specialist. You may be able to decrease the volume of fluid used if output is dirty water or, if output has consistency, may need to alter the regimen used.
- In some children, despite everyone’s best efforts to find and adhere to a suitable washout regimen, soiling between washouts continues to be a problem.
Child is experiencing abdominal cramps during washout
Action needed:
- Reduce the speed of the washout.
- Ensure the sodium chloride is warm enough.
Child appears constipated
It is possible to get constipated even if using washouts daily.
Action needed:
- Administer 1ml per kg of body weight of oil (Arachis oil enema can be prescribed for children if no history of nut allergy but if any history of nut allergy, use sunflower oil) to soften the stool.
- Leave for a minimum of four hours but preferably until the next washout.
An exceptional circumstance has occurred (for example child will be on a flight) and washout is missed
Action needed:
If evening washout is missed, administer 1ml per kg of Arachis oil or equivalent (see above) the following morning then continue with evening washout as normal.
Unable to pass the intermittent catheter through the ACE channel
Following surgery, it is not uncommon for the stoma to shrink a little (stenosis) resulting in difficulty passing the catheter.
Action needed:
- Inserting the catheter twice daily and / or using an ACE stopper should prevent this.
- If stenosis does occur, use a smaller size catheter for a one to two days, then go back to the normal size. If this fails continue using the size smaller catheter but contact the nurse specialist to discuss use of tapered tip catheters.
- Occasionally an indwelling catheter needs to be reinserted for one to two weeks or, very occasionally, dilation (widening) of the tract is necessary under general anaesthetic.
Child develops gastroenteritis
Action needed:
- If the child is well enough, continue ACE washouts to help clear the bacteria / virus.
- If the child is not well enough, refer to the ‘missed washout’ regimen.
Follow up
Your child will be re-admitted approximately six weeks after their initial surgery; the date for this will be arranged with you before discharge.
Once your child has commenced intermittent catheterisation via the ACE, they will be reviewed in the outpatient clinic approximately three months later. You will receive a letter in the post giving details of the appointment. Please ensure you telephone the clinic if you are unable to attend.
Chaperoning
During your child’s hospital visits your child will need to be examined to help diagnosis and to plan care. Examination may take place before, during and after treatment. It is performed by trained members of staff and will always be explained to you beforehand. A chaperone is a separate member of staff who is present during the examination. The role of the chaperone is to provide practical assistance with the examination and to provide support to the child, family member / carer and to the person examining.
Contacts and queries, concerns or questions?
Clinical nurse specialists: 01223 586973 (08:00 to 18:00 Monday to Friday) Ward
. . . . . . . . . . . . . . . . . . . . . . . . . . .
Your child’s community children’s nurse
. . . . . . . . . . . . . . . . . . . . . . .
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/

