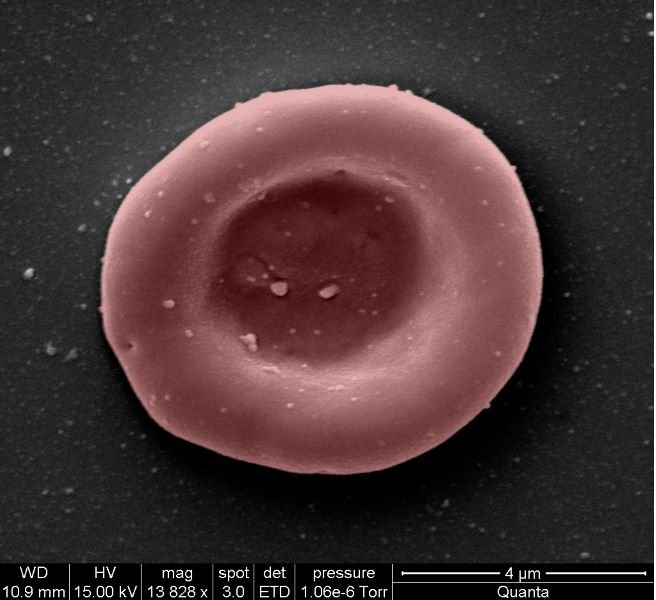
An Addenbrooke's team is involved in a pioneering clinical trial, growing red blood cells in a lab and transfusing them into another person.
It's hoped the RESTORE trial will help revolutionise treatment for people where it’s almost impossible to find matching blood.
Tiny amounts, equivalent to a couple of spoonfuls, are being tested to see how it performs inside the body.
In the trial, manufactured blood cells are grown from stem cells from donors.

If our trial is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future
Professor Cedric Ghevaert, consultant haematologist, at CUH.
Two people have so far been transfused with the lab grown red cells.
They were closely monitored and no untoward side effects were reported and they are well and healthy.
Professor Cedric Ghevaert, is chief investigator on the trial and a consultant haematologist at CUH and NHS Blood and Transplant. He said:
"We hope our lab-grown red blood cells will last longer than those that come from blood donors. If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future, helping transform their care."

The bulk of blood transfusions will always rely on people regularly rolling up their sleeves to donate.
But the ultimate goal is to manufacture vital, but ultra-rare, blood groups that are hard to get hold of.
These are necessary for people who depend on regular blood transfusions for conditions such as sickle cell anaemia.
RESTORE trial
The RESTORE trial is a joint research initiative by NHS Blood and Transplant and the University of Bristol, working with Cambridge University Hospitals NHS Foundation Trust (CUH), the University of Cambridge and Guy’s and St Thomas’ NHS Foundation Trust, NIHR Cambridge Clinical Research Facility. It is part-funded by a National Institute for Health and Care Research grant.
The trial is studying the lifespan of the lab grown cells compared with infusions of standard red blood cells from the same donor.
The lab-grown blood cells are all fresh, so the trial team expect them to perform better than a similar transfusion of standard donated red cells, which contains cells of varying ages.
Additionally, if manufactured cells last longer in the body, patients who regularly need blood may not need transfusions as often. That would reduce iron overload from frequent blood transfusions, which can lead to serious complications.
The trial is the first step towards making lab grown red blood cells available as a future clinical product.

Dr Rebecca Cardigan is co-chief investigator for the trial, head of component development for NHS Blood & Transplant and affiliated lecturer at the University of Cambridge. She said:
It’s really fantastic that we are now able to grow enough red cells to medical grade to allow this trial to commence.
Dr Rebecca Cardigan
New volunteers for the trial will be recruited through the NIHR Cambridge BioResource and study clinical team and will receive their infusions in the NIHR and Wellcome Trust Clinical Research Facility at Addenbrooke’s.
A minimum of 10 participants will receive two mini transfusions at least four months apart, one of standard donated red cells and one of lab grown red cells, to find out if the young red blood cells made in the laboratory last longer than cells made in the body.
Further trials are needed before clinical use, but this research marks a significant step in using lab grown red blood cells to improve treatment for patients with rare blood types or people with complex transfusion needs.

